Background
Cardiovascular diseases and advanced age are recognized risk factors for atrial fibrillation (AF). Recent evidence supports a prognostic benefit from rhythm control strategies, primarily achieved through catheter ablation. However, a high comorbidity burden may influence efficacy and the incidence of cardiovascular events following pulmonary vein isolation (PVI).
Methods
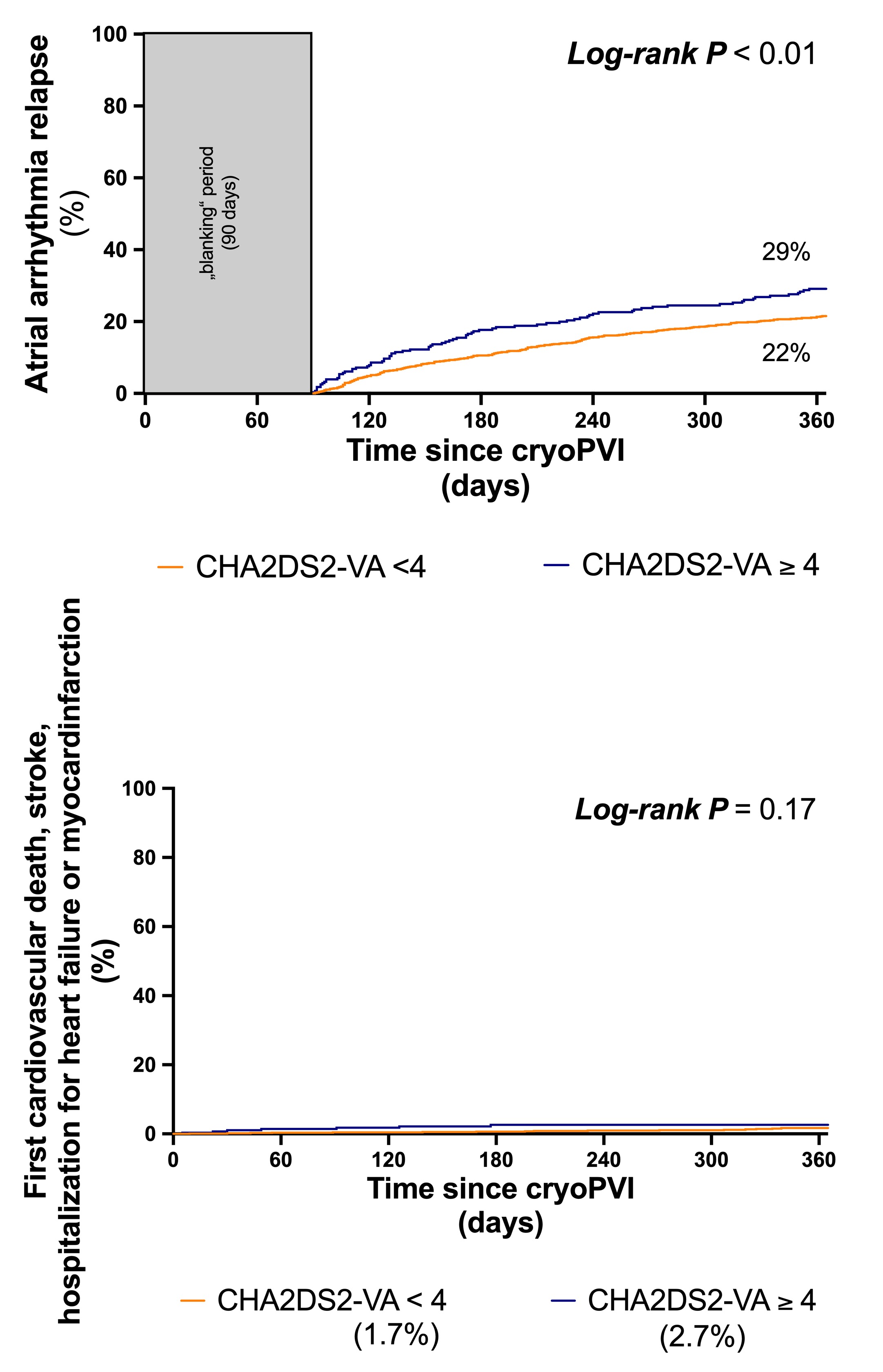
This prospective study included consecutive AF patients who underwent first-time PVI with cryoballoon (cryoPVI) between 2018 and 2024. Patients were grouped based on comorbidity burden (CHA2DS2-VA score <4 or ≥4). CryoPVI was conducted using a standardized protocol, with follow-up assessments at 3, 6, and 12 months. The primary efficacy endpoint was symptomatic atrial arrhythmia relapse, while the secondary endpoint included a composite of cardiovascular death, stroke or transient ischemic attack, and hospitalization for heart failure or acute coronary syndrome, consistent with the EAST-AFNET4 trial criteria. Periprocedural parameters were also evaluated.
Results
A total of 1402 patients were included, of whom 281 (20%) had a CHA2DS2-VA score ≥4. Mean follow-up duration was 11±3 months. Patients with CHA2DS2-VA ≥4 were older (77 vs. 67 years; P<0.0001) and had a higher prevalence of persistent AF (48% vs. 37%, P=0.0008), hypertension (89% vs. 61%; P<0.0001), diabetes (33% vs. 7%; P<0.0001), coronary artery disease (48% vs. 12%; P<0.0001), and prior stroke (26% vs. 2%; P<0.0001). At 12 months, atrial arrhythmia relapse was significantly higher in patients with a high comorbidity burden (29% vs. 22%, hazard ratio 1.44; 95% confidence interval 1.1–1.9; log-rank P<0.01). No significant difference was observed for the secondary endpoint (2.7% vs. 1.7%, hazard ratio 1.9; 95% confidence interval 0.65–5.23; log-rank P=0.17). Procedural parameters did not differ between groups.
Summary & Conclusion
CryoPVI proves to be less effective in patients with high comorbidity burden, however it does not increase the likelihood of adverse cardiovascular events.