Background: The Systemic Immune-Inflammation Index (SII) is a novel composite biomarker that integrates neutrophil, lymphocyte, and platelet counts, reflecting both systemic inflammatory response and immune activation. While the SII has demonstrated prognostic significance in various clinical settings, its prognostic value in patients undergoing transcatheter aortic valve implantation (TAVI) remains poorly understood.
Methods: This retrospective cohort study, conducted at a single tertiary cardiac center (TUM University Hospital, German Heart Center), analyzed patients (n=1,254) undergoing transcatheter aortic valve implantation (TAVI) for severe aortic stenosis. Preprocedural SII was calculated using the formula: SII = [platelet count × neutrophil count] / lymphocyte count. The primary endpoint was 1-year MACE after TAVI. Secondary endpoints were all-cause mortality, stroke and CHF (hospitalization for heart failure) at 1 year. Patients were stratified into tertiles based on preprocedural SII levels. GLM was performed to identify predictors of SII and multivariable Cox regression analysis was performed to identify predictors of MACE adjusting for baseline, clinical and procedural characteristics.
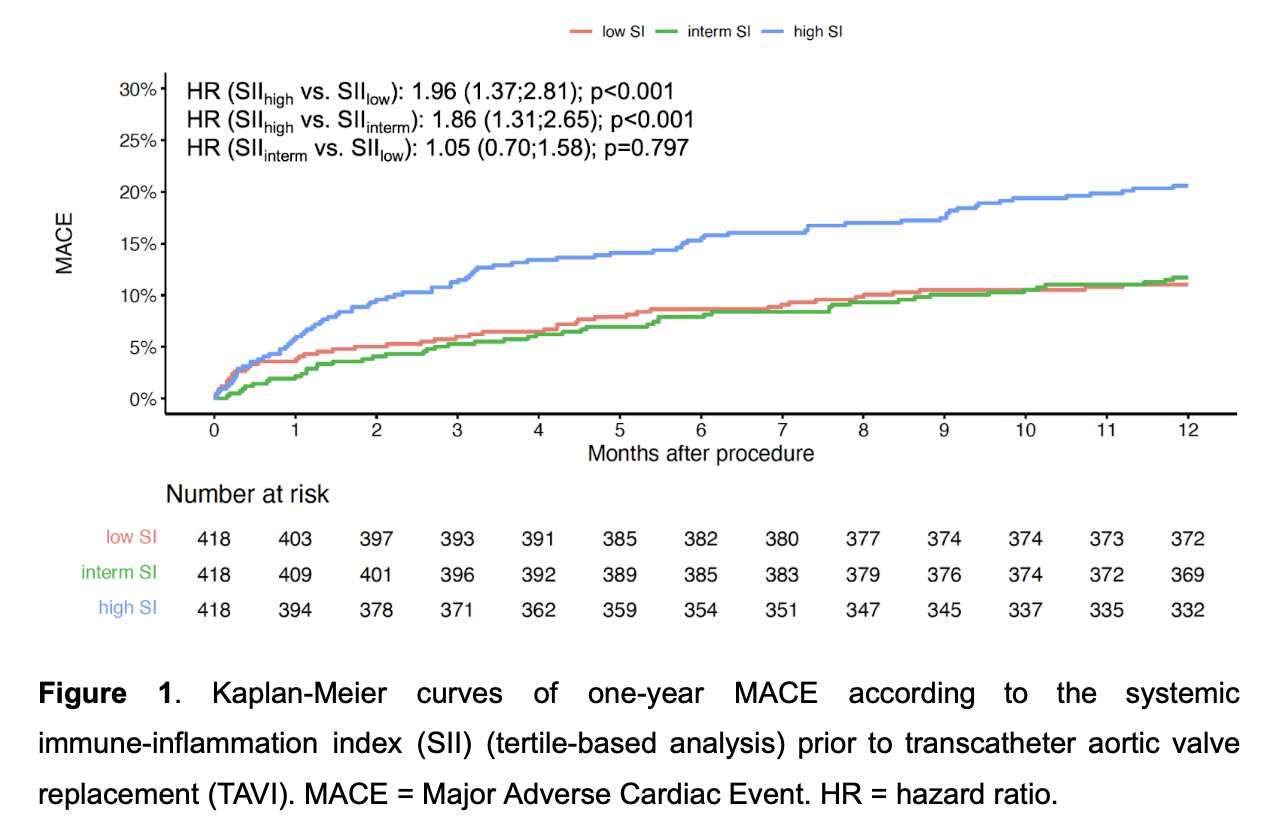
Results: In the GLM, age (estimates 16.13, p=0.013) and CRP (estimates 23.31, p<0.001) significantly correlated with SII whereas lower AS mean gradient (estimates -7.23, p=0.022) and Hb (estimates -60.85, p=0.011) showed negative correlation with SII. At 1 year, MACE in the overall population was 14.4% (181/1254). Specifically, 11.0% (46/418) in the low SII group, 11.7% (49/418) in the intermediate SII group and 20.6% (86/418) in the high SII group. In the univariable Cox regression analysis, the incidence of MACE was significantly higher in patients within the high SII group compared to both the intermediate SII group (HR 1.86 [1.31;2.65], p<0.001) and low SII group (HR 1.96 [1.37;2.81], p<0.001). After multivariate adjustment, SII remained a significant predictor of MACE, when used as a continuous variable (HR 1.0001 [1.00001;1.00002], p=0.020).
Conclusion: In this study, the preprocedural SII demonstrated significant value as a predictor of MACE in a large cohort of patients undergoing TAVI. These findings suggest that SII, as a readily available and cost-effective biomarker, may enhance current risk stratification models and help identify high-risk patients prior to TAVI.