Background:
Radiofrequency-guided catheter ablation (RFCA) is a well-established technique for treating arrhythmias caused by accessory pathways. However, ablation of septal accessory pathways (SAPs) presents unique anatomical challenges, requiring alternative access strategies in certain cases.
Aims:
This study aimed to evaluate the safety and efficacy of RFCA for SAPs with a focus on outcomes related to standard and alternative access approaches.
Methods:
A total of 116 patients (mean age 35.6 ± 17.5 years, 57% male) were enrolled that had undergone RFCA for SAPs. SAP-localizations were defined by the Smart-WPW O’clock scheme (Figure 1). Standard access via the vena femoralis was used. If standard access failed, alternative routes via the left vena subclavia/ right vena jugularis or non-coronary cusp in the aorta were applied (Figure 2).
Results:
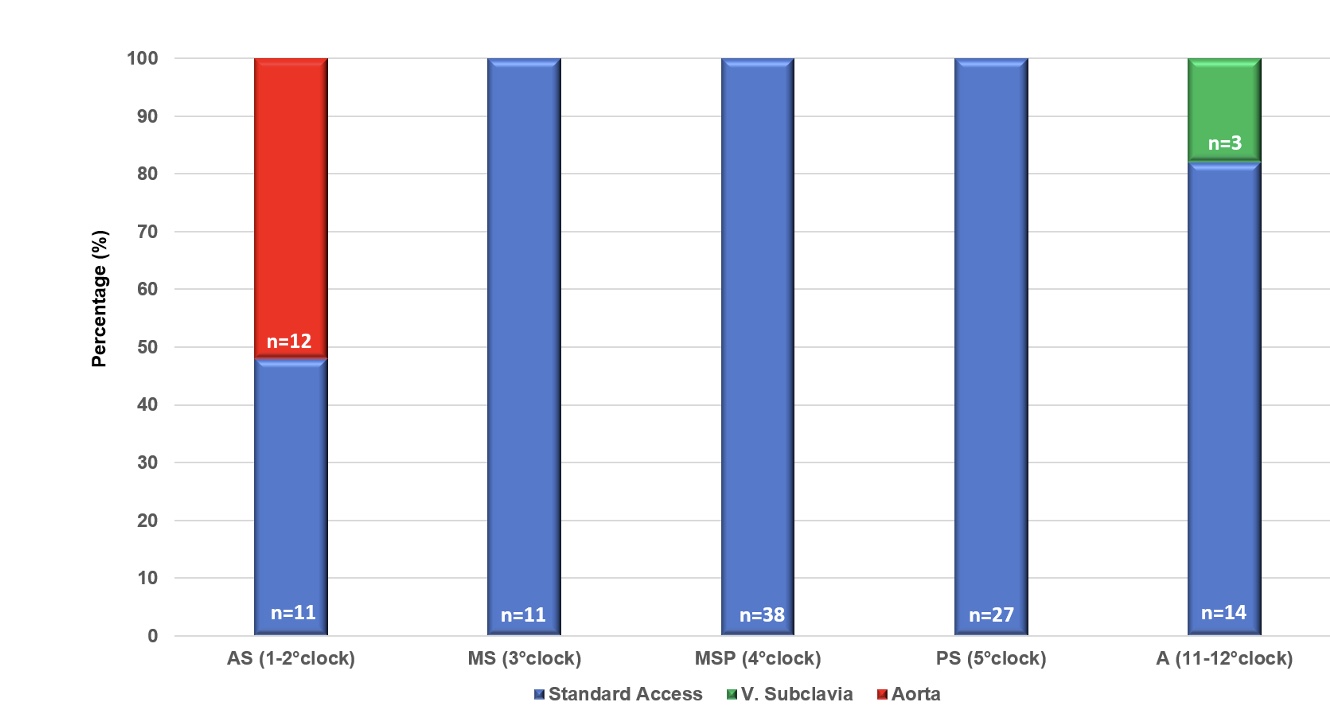
The success rate for RFCA was 100% (n=116). Standard access was applied in all patients (n=116, 100%). An additional alternative access was required in 15/116 patients (13%). For anteroseptal pathways (AS 1-2°clock) (n=23/116, 20%) standard access was sufficient in 11/23 cases (48%). An alternative approach via the non-coronary cusp was necessary in 12/23 patients (52%). For midseptal-(MS 3 O’clock: n=11/11, 100%), midseptal-posterior (MSP 4 O’clock: n=38/38, 100%) and postero-septal pathways (PS 5 O’clock: n=27/27, 100%) standard access was sufficient in all patients. Anterior pathways (A 11-12 O’clock) were successfully ablated through standard access in 14/17 patients (82%). An alternative access via the vena subclavia was required in 3/17 cases (18%) (Figure 3). Complication rates amounted to 2% (2/116) as two patients with anteroseptal-pathways presented with a right bundle branch block after using standard access.
Conclusion:
RFCA for SAPs demonstrates high safety and efficacy, with tailored access strategies optimizing outcomes based on pathway location. For anterior pathways (A 11-12 O’clock), an alternative access via the left vena subclavia/right vena jugularis and for anteroseptal pathways (AS 1-2 O’clock) access via the non-coronary cusp in the aorta seem to provide effective solutions for challenging cases. Further studies are warranted to validate these findings and refine procedural approaches.
Key words: septal WPW ablation; septal accessory pathway; anteroseptal accessory pathway; His accessory pathway.
Figure 1: Smart-WPW O’clock scheme (Khalaph et al, SMART-WPW Algorithm, Heart Rhythm 2025)
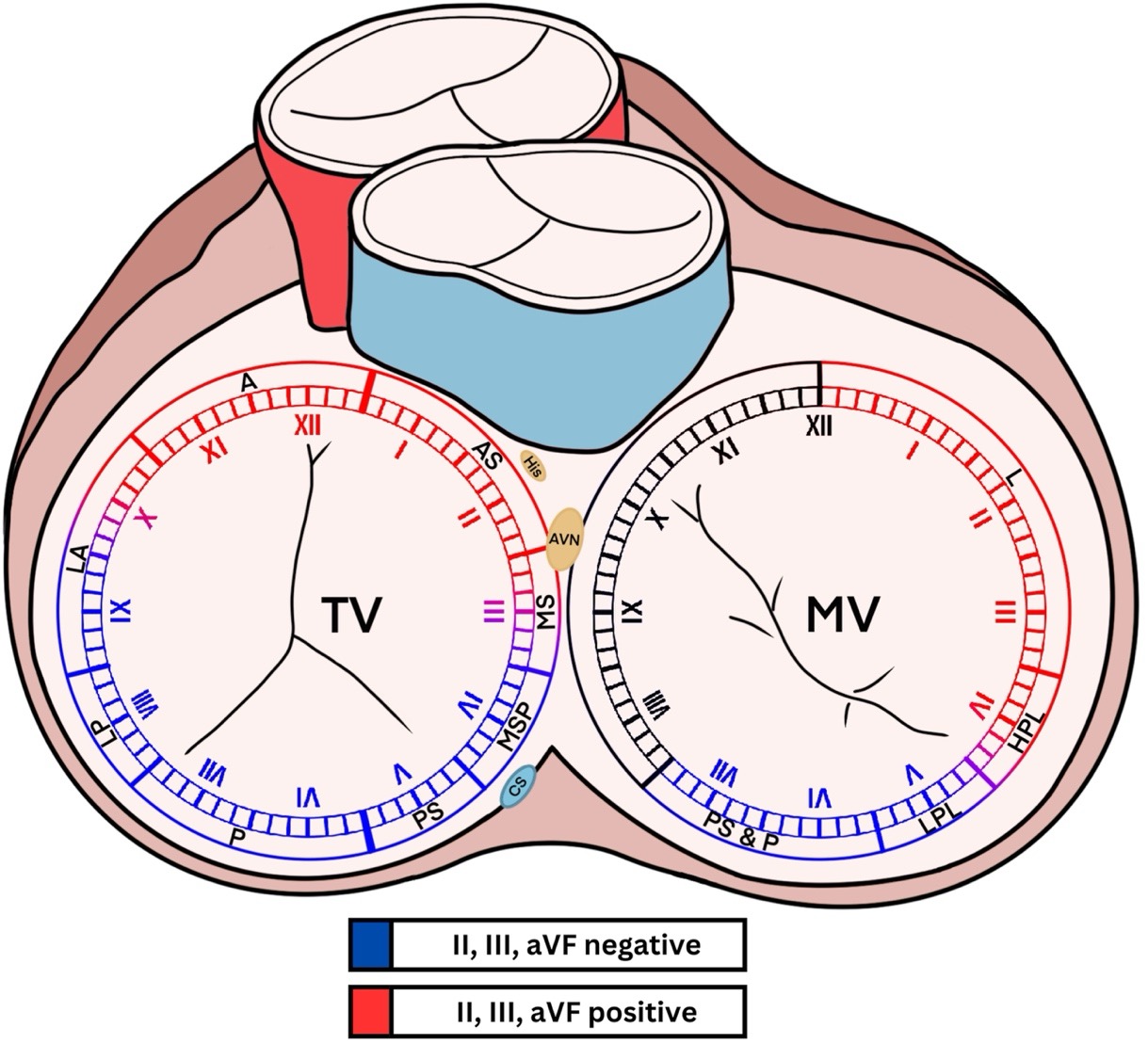
Figure 2: Alternative Access routes for Septal Accessory Pathways.
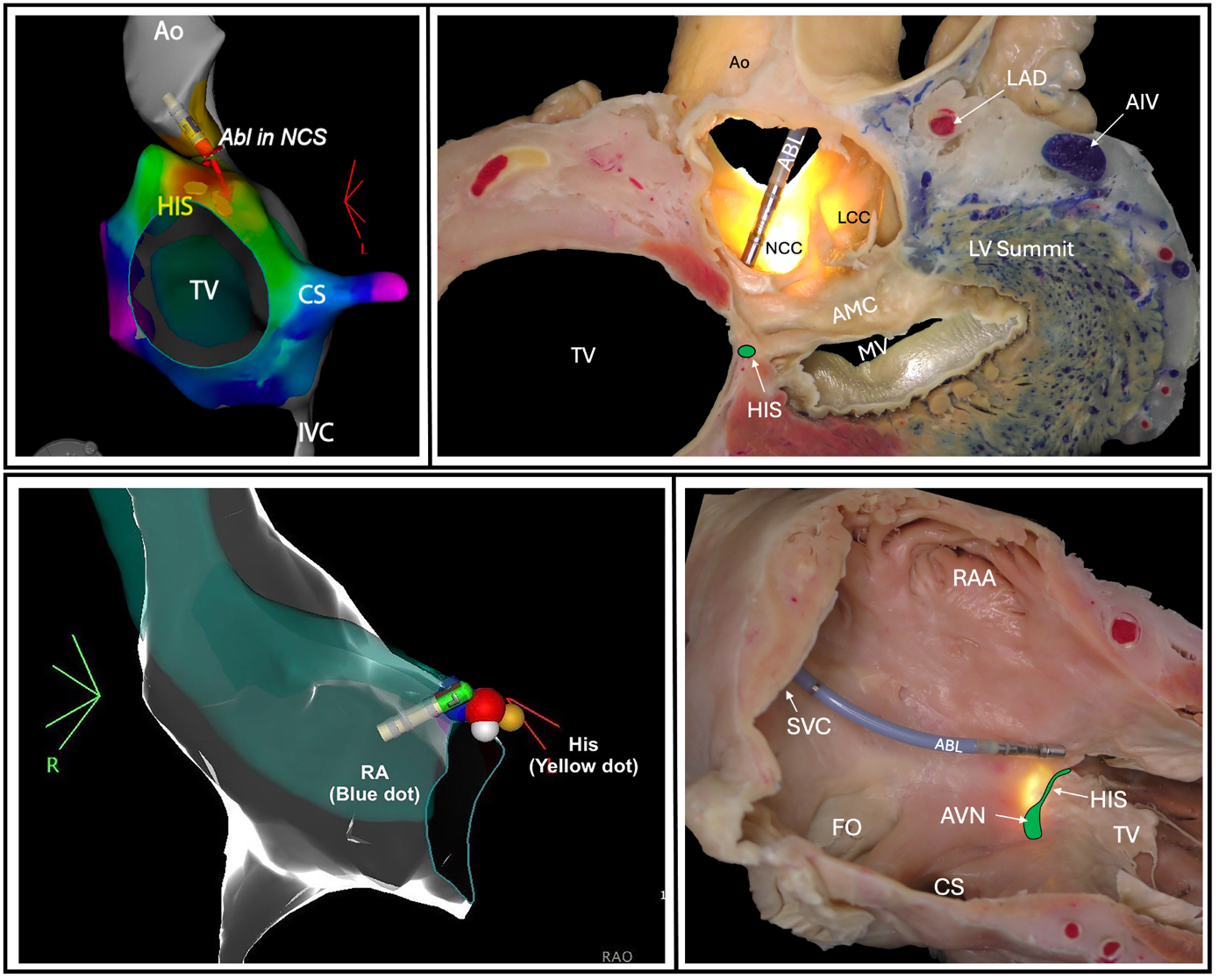
Figure 3: Access routes for Septal Accessory Pathways.
SAP-localizations were defined by the Smart-WPW O’clock scheme. AS, antero-septal; MS, midseptal; MSP, midseptal-posterior; PS, posteroseptal; A, anterior.