Background: A tapered left ventricular outflow tract (LVOT) may influence outcomes in transcatheter aortic valve implantation (TAVI), especially regarding valve positioning and conduction disturbances. While this is established in cases of pure aortic regurgitation and stenosis with balloon-expandable valves, its effect in native high-grade aortic stenosis (AVS) using self-expandable (SE) valves remains unclear. This study evaluated the impact of tapered LVOT morphology on procedural outcomes with the SE NAVITOR prosthesis.
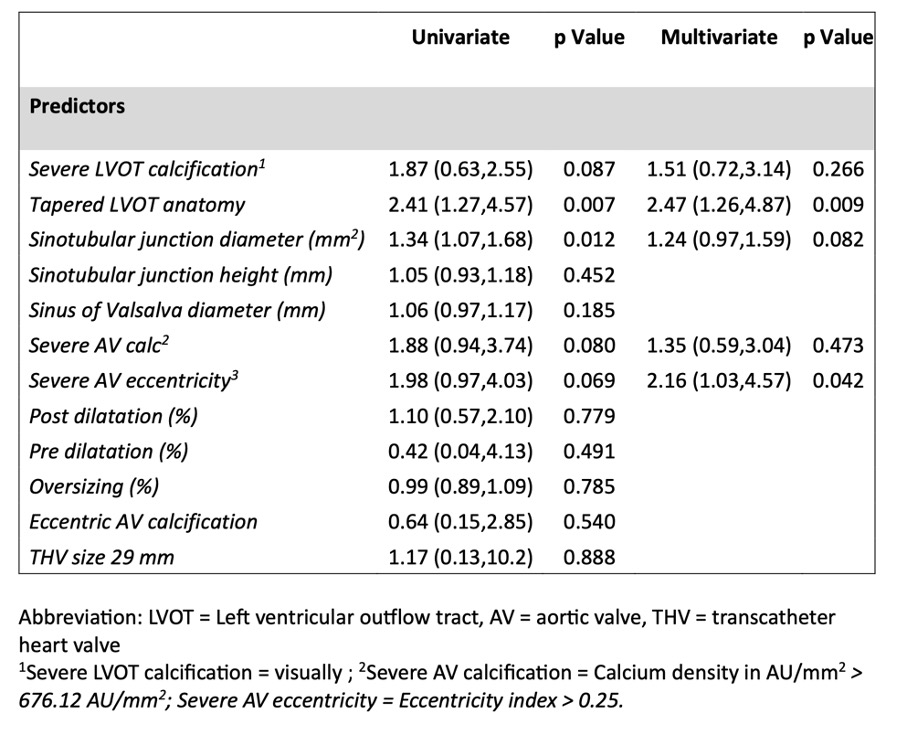
Methods: Between June 2021 and April 2025, 354 patients with severe native AVS underwent TAVI using the SE NAVITOR (n=313) or NAVITOR Vision (n=41). Patients were stratified based on LVOT morphology (tapered vs. non-tapered), see Figure 1. Clinical and hemodynamic outcomes, including incomplete device migration and embolisation, were compared between groups.
Results: Technical success (96.9% tapered vs. 97.8% non-tapered, p=0.727) and device success (92.9% vs. 89.4%, p=0.373) were similarly high. Incomplete device migration occurred significantly more often in patients with a tapered LVOT (18.9% vs. 6.6%, p=0.001). Rates of embolisation (0.8% vs. 2.6%, p=0.429) and Valve-in-Valve procedures (0.8% vs. 1.8%, p=0.658) were overall rare. Multivariate logistic regression identified a tapered LVOT morphology (OR 2.47; 95% CI 1.26–4.87; p=0.009) and severe aortic valve eccentricity (OR 2.16; 95% CI 1.03–4.57; p=0.042) as independent predictors for incomplete migration and embolisation, see Table 1 and Figure 2. The rate of permanent pacemaker implantation was comparable (18.0% vs. 17.4%, p=1.000).
Conclusion: TAVI with the SE NAVITOR prosthesis demonstrated high procedural success across anatomical subgroups. However, a tapered LVOT was associated with a significantly increased risk of incomplete device migration. Alongside severe valve eccentricity, it independently predicted migration-related events. These findings highlight the critical importance of preprocedural anatomical assessment, particularly LVOT morphology, in optimizing outcomes for TAVI in native AVS.
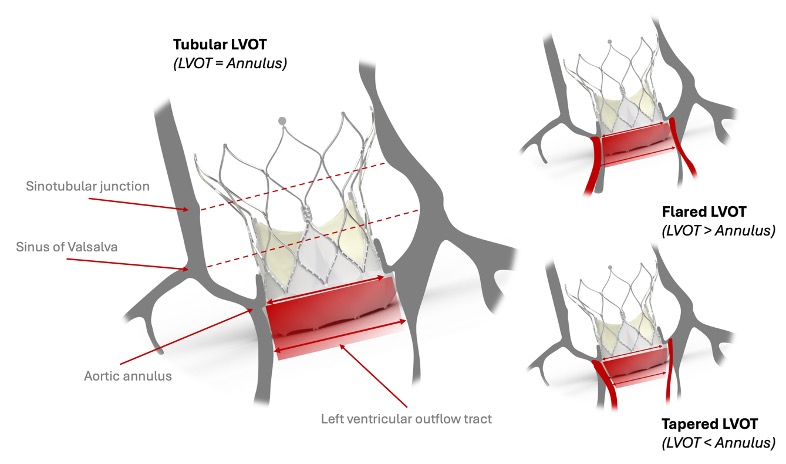
Figure 1: Anatomical classification of the LVOT was based on the LVOT-to-annulus area ratio, with tapered (< 0.85), tubular (0.85–1.1), and flared (> 1.1) configurations [2].
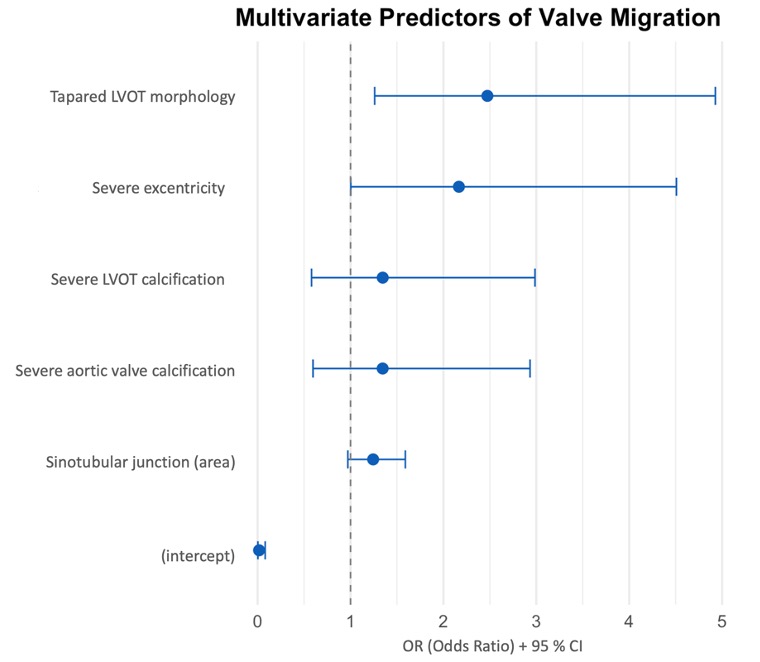
Figure 2: Multivariate logistic regression model for the prediction of incomplete prosthesis migration and embolization
Table 1: Multivariate Regression model for incomplete prosthesis migration and device embolization