Background: Pulsed field ablation (PFA) is a novel non-thermal ablation technique for pulmonary vein isolation (PVI) in atrial fibrillation. This study investigates the association between post-procedural high-sensitivity troponin T levels and arrhythmia recurrence following PFA-PVI.
Aim: This study aims to evaluate whether high-sensitivity troponin T levels measured after pulsed field ablation can serve as a biomarker to predict atrial fibrillation recurrence during follow-up, thereby supporting individualized risk stratification and monitoring strategies.
Methods: We conducted a retrospective single-center analysis of 114 patients who underwent a first pulmonary vein Isolation (first-PVI) for atrial fibrillation with pulsed field ablation between May 2024 and January 2025. Post-procedural high-sensitivity troponin T levels were measured, and clinical follow-up data were analysed for arrhythmia recurrence (atrial fibrillation and atrial flutter).
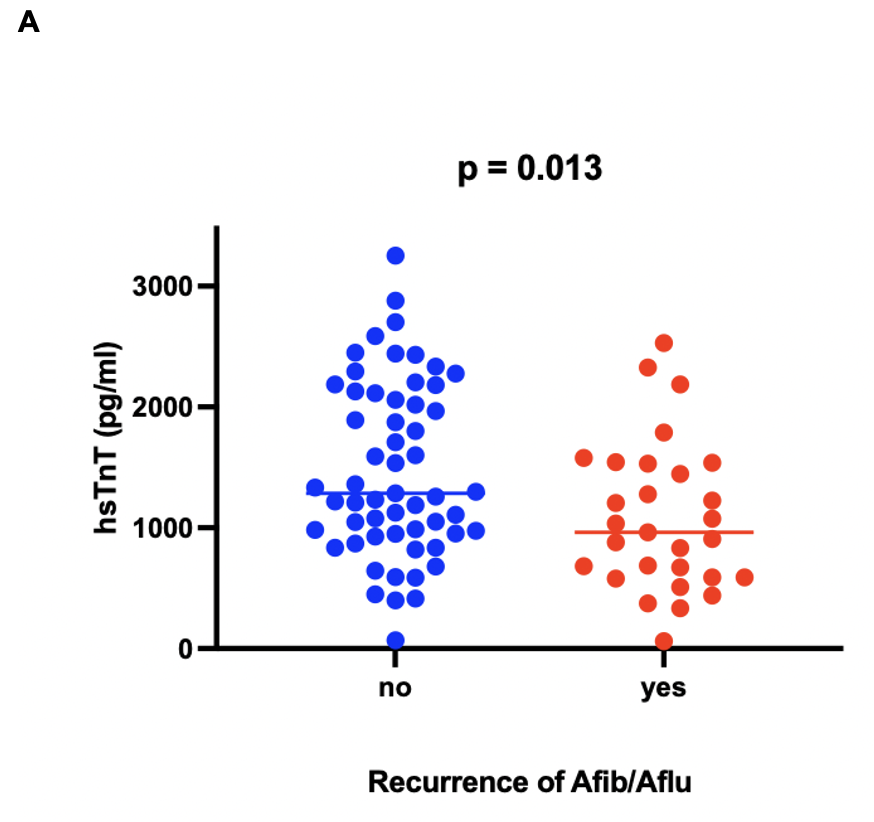
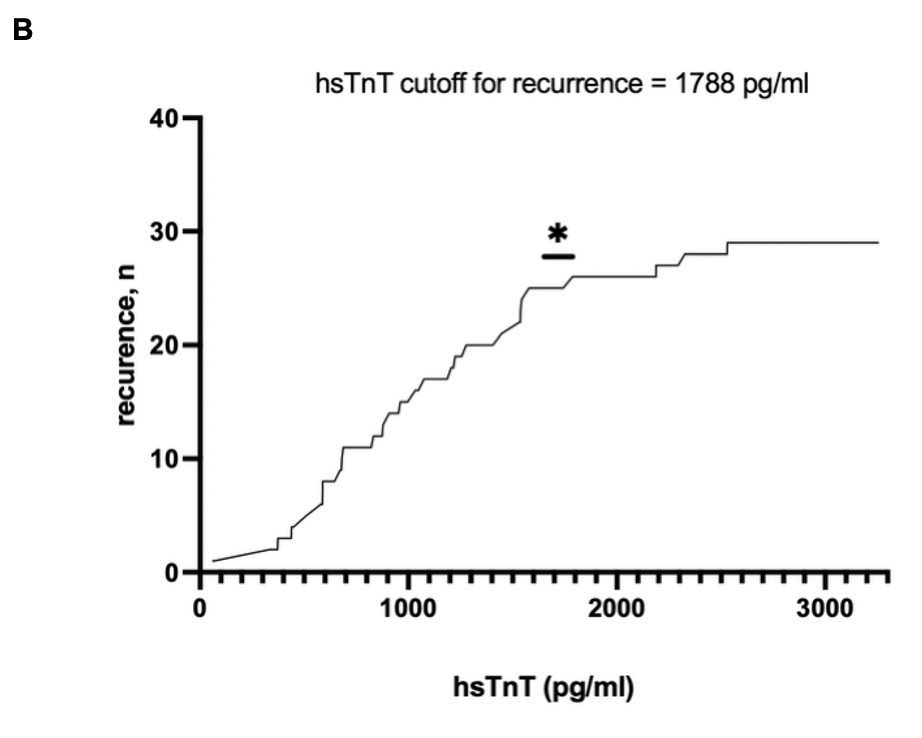
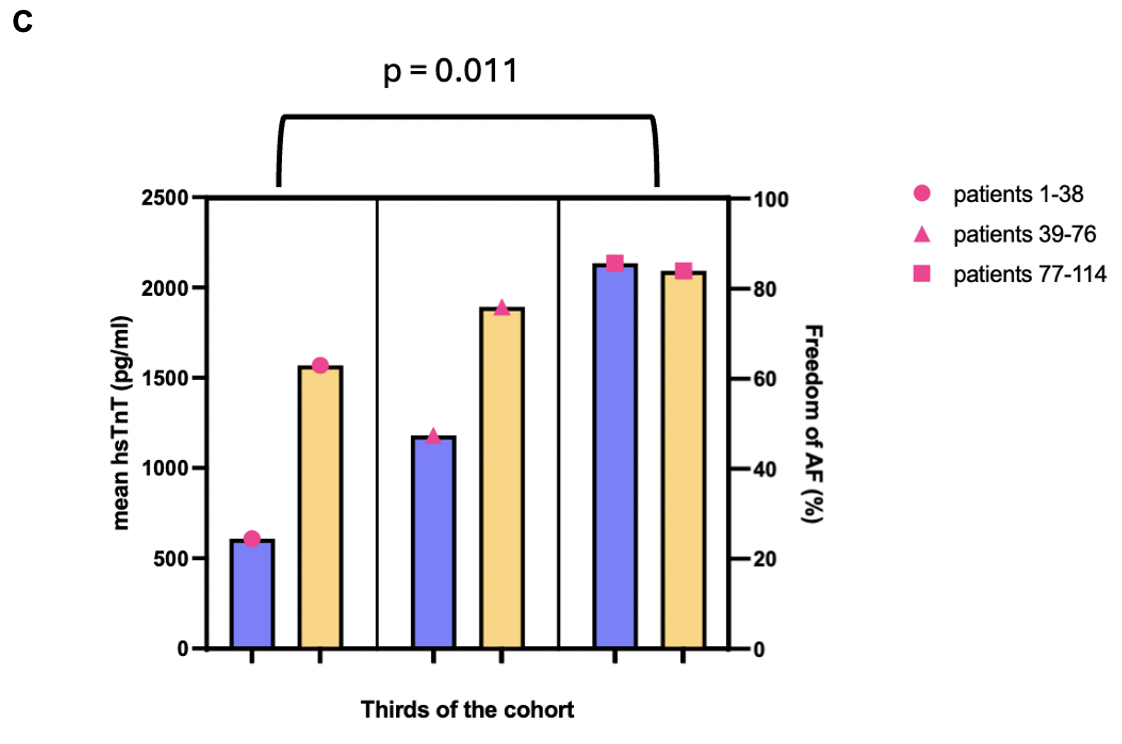
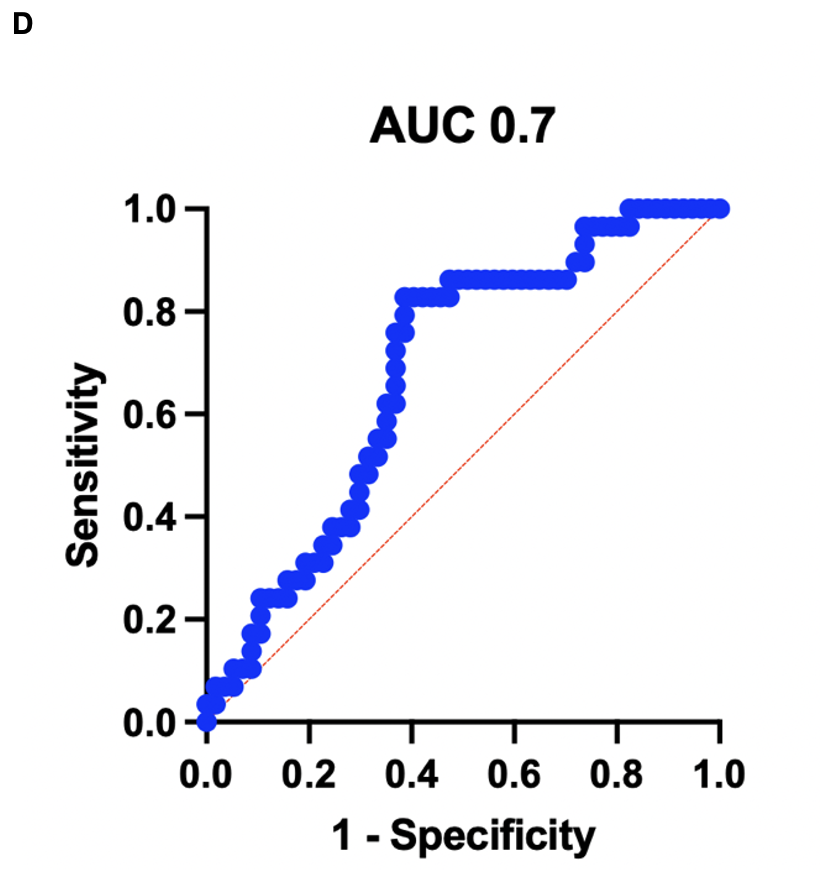
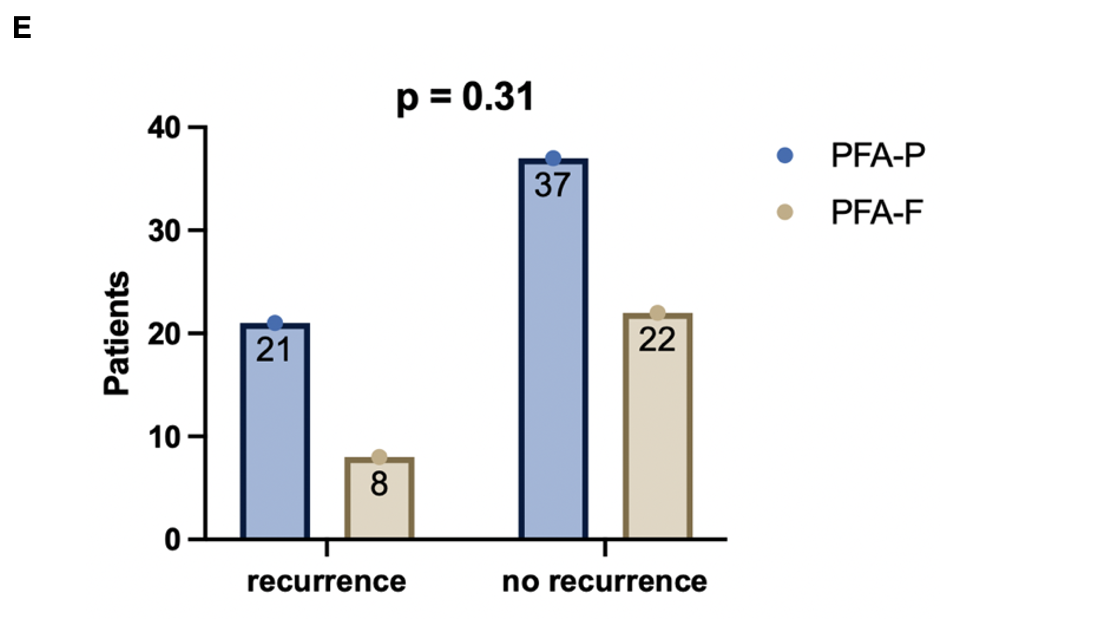
Results: A total of 114 patients undergoing first-time pulmonary vein isolation using pulsed field ablation were included in this retrospective analysis. Of these, 71 patients were treated with the Medtronic™ PulseSelect catheter (PFA-P) and 43 with the Boston Scientific™ Farapulse system (PFA-F). The mean age was 68 ±9 years, and 59% of patients were male. The average BMI was 29 ±3.6 kg/m². Paroxysmal atrial fibrillation was present in 59% of the cohort. The mean CHA₂DS₂-VASc and HAS-BLED scores were 2.8 and 1.7, respectively. High-sensitivity troponin T (hs-TnT) levels were measured before ablation, as well as on post-procedural days 1 and 2; the highest value per patient was included in the analysis. Follow-up data were available for 88 patients (77%), among whom 29 experienced atrial fibrillation (Afib) or atrial flutter (AFlu) recurrence in a median follow-up time of 103 days. Interestingly, patients without recurrence had significantly higher hs-TnT levels compared to those with Afib/Aflu recurrence (median 1286 vs 962 pg/ml p = 0.013). The cutoff for the recurrence of atrial fibrillation or flutter was calculated to be 1788 pg/ml. Next, the cohort of 114 patients was divided into 3 numerically equally distributed groups with ascending troponin and the incidence of Afib/Aflu recurrences was compared between the groups. The mean hsTropT value in the respective groups was 608, 1180 and 2134 pg/ml. There was a statistically relevant difference in the occurrence of Afib/Aflu recurrences between the first and third groups (p = 0.011). These findings suggest an inverse relationship between post-ablation hs-TnT levels and arrhythmia recurrence.
Regarding recurrence rates we observed no statistically significant difference between the two PFA modalities (PFA-P 36% vs. PFA-F 27%, p = 0.31). Also, the mean hsTnT and CK-MB did not differ statistically significant between the two modality groups (mean hsTnT 1393 Vs 1168 pg/ml p = 0.17 and mean CK-MB 68 Vs 39 U/L p = 0.35 for PFA-P and PFA-F respectively).
Conclusion: In this single-center study, higher post-procedural high-sensitivity troponin T levels were associated with a lower risk of atrial fibrillation recurrence following pulsed field ablation. This inverse correlation may reflect more effective lesion formation. The type of PFA system used did not significantly influence outcomes. Further prospective studies are warranted to validate hs-TnT as a potential biomarker for ablation efficacy.