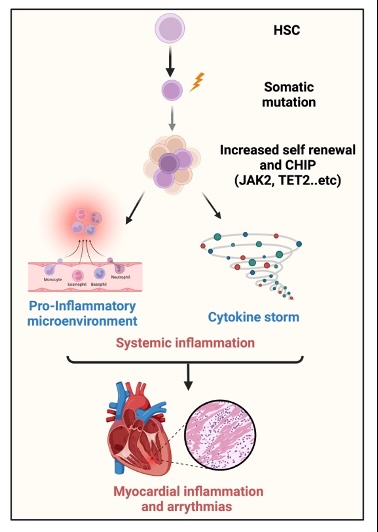
Objective: Cytopenia—defined as a reduction in one or more blood cell lineages—has been increasingly recognized as an independent risk factor for adverse cardiovascular outcomes. In patients with heart rhythm disorders, the prevalence and clinical implications of cytopenia remain largely unexplored. This study aimed to evaluate the prevalence and hematological patterns of cytopenia in a cohort of patients undergoing rhythmological evaluation. In a second step, we focused on clonal cytopenia of undetermined significance (CCUS), a condition characterized by somatic mutations in hematopoietic progenitor cells in the absence of overt hematologic malignancy. CCUS is considered a potential precursor to hematologic neoplasms and may contribute to cardiovascular disease via chronic inflammatory mechanisms. Our goal was to determine how frequently CCUS occurs within the cytopenic subgroup.(Figure 1).
Methods: To evaluate the prevalence of cytopenia, we retrospectively reviewed all patients treated at the Department of Rhythmology, University Heart Center Lübeck during 2021 and 2022. Patients diagnosed with anemia (hemoglobin <10 g/dL), thrombocytopenia (platelet count <100 × 10^9/L), or leukocytopenia (absolute neutrophil count <1 × 10^9/L or absolute leukocyte count < 2 × 10^9/L) were classified as cytopenic. Those with cytopenia due to alternative causes—such as acute bleeding, substrate deficiency, sepsis, or active oncological diseases—were excluded. In a subsequent step, cytopenic patients are now contacted, and after obtaining written informed consent, they undergo genetic testing for TET2 and JAK2 mutations. Patients, who didn’t consent to the genetic testing will be excluded from further analysis.
Results: As we analyzed the first 1683 patients, we found that initially 32.1% exhibited cytopenia. After excluding patients with alternative causes of cytopenia, the proportion decreased to 11,7% of the total cohort. Among these patients, 46.1% were solely anemic, 1.8% had isolated leukopenia, 25.5% were thrombocytopenic, and in 28.3%, more than one cell line was affected. When compared to the overall cohort, patients with heart failure (11.7% vs. 24.7%, p < 0.001), atrial tachycardia (11.7% vs. 15.98%, p = 0,0312), and ventricular tachycardia or ventricular fibrillation (11.7% vs. 24.6%, p = 0.011) were significantly more likely to exhibit cytopenia. Although not statistically significant, patients with premature ventricular beats appeared less likely to be cytopenic (11.7% vs. 6.25%). The evaluation of clonal cytopenia in this cohort is still ongoing.
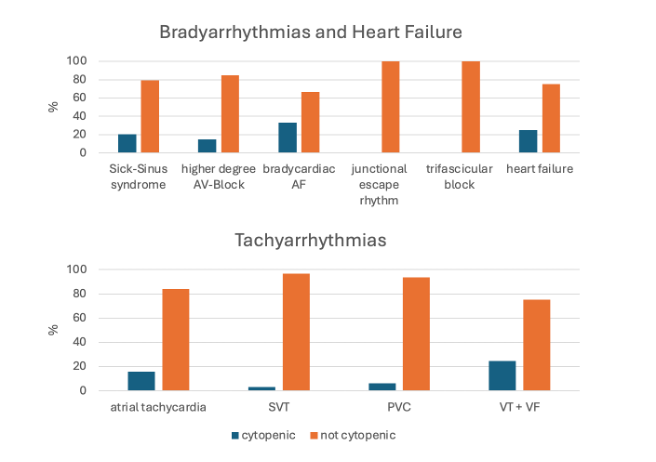
Figure 2 Cytopenic propotion in different entities: AF: atrial fibrillation, SVT: supraventricular tachycardia including AVNRT and AVRT, PCV: premature ventricular capture, VT: ventricular tachycardia, VF: ventricular fibrillation
Discussion: This is the first study to assess the prevalence of cytopenia in patients with heart rhythm disorders. We found unexplained cytopenia in 11.7% of patients, especially those with heart failure, ventricular arrhythmias, and atrial tachycardia—higher than in the general population, but lower than in high-risk groups like TAVI patients. Cytopenia may reflect not only systemic disease burden but also contribute to arrhythmogenesis through inflammatory or fibrotic pathways. Given the role of clonal hematopoiesis (e.g., CHIP, CCUS) in cardiovascular risk, hematologic screening could help identify arrhythmia patients at higher risk and guide management.
