BACKGROUND:
Bland-White-Garland syndrome (BWGS) is a rare coronary anomaly with an incidence of 1 in 300,000 live births and is characterized by an anomalous origin of the left coronary artery from the pulmonary artery. Most patients present within the first year of life. Without surgical correction, up to 90% may not survive beyond infancy. The pathophysiology involves a "coronary steal" phenomenon, where deoxygenated blood from the high-pressure right coronary artery (RCA) flows via well-developed collaterals into the low-pressure left coronary artery (LCA) system and then drains into the main pulmonary artery, leading to chronic myocardial hypoperfusion. Manifestation in adults occurs only in rare cases, presenting symptoms of chronic myocardial ischemia, arrhythmias, heart failure, or even sudden cardiac death.
CASE DESCRIPTION:
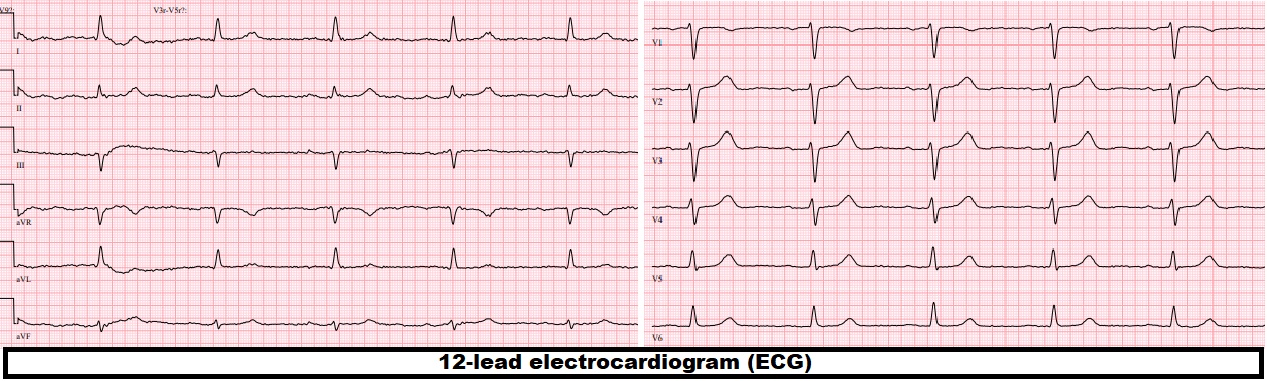
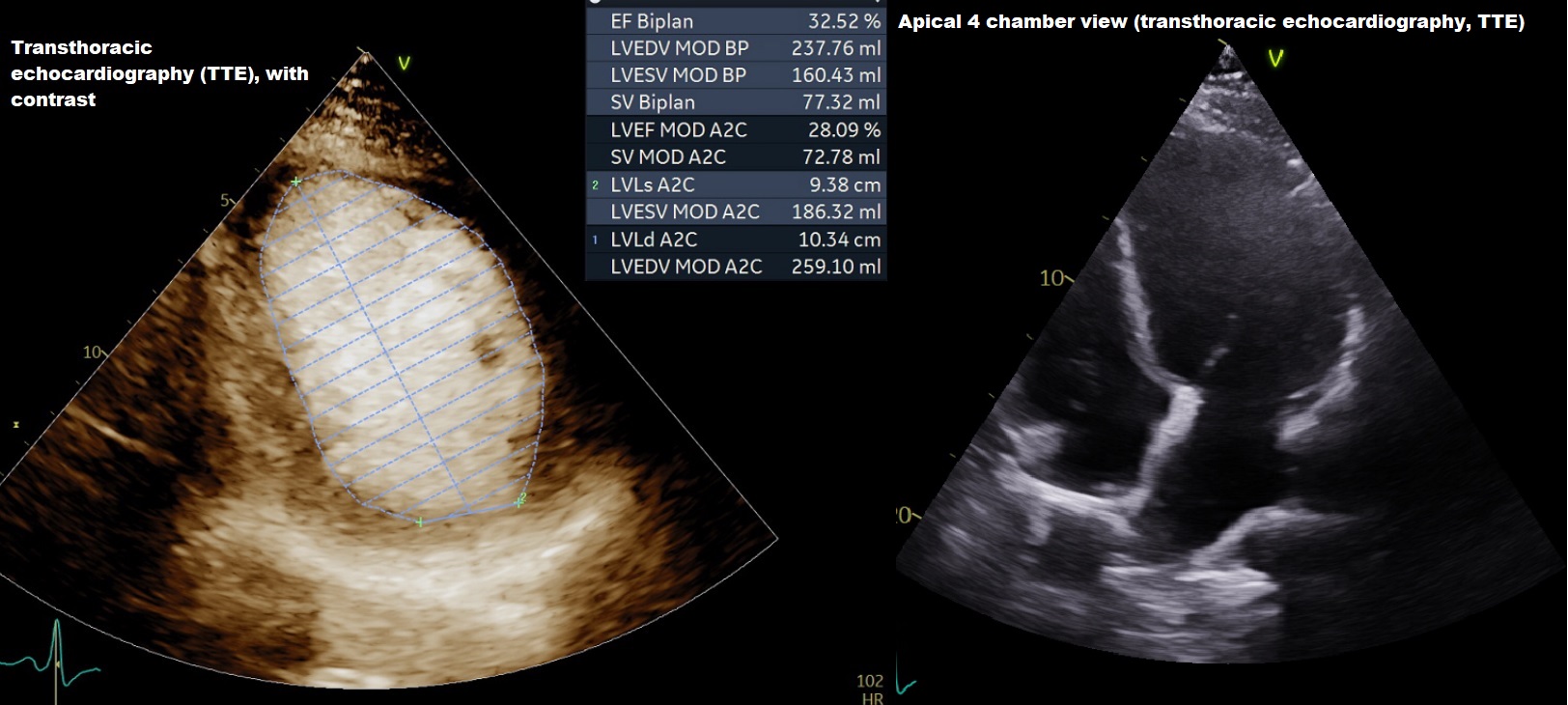
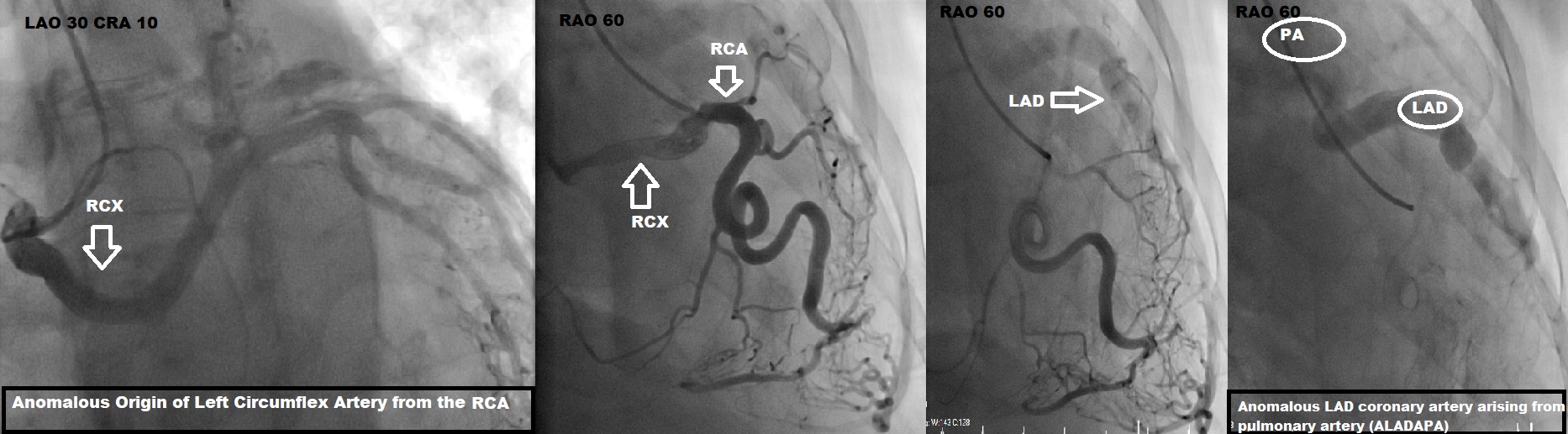
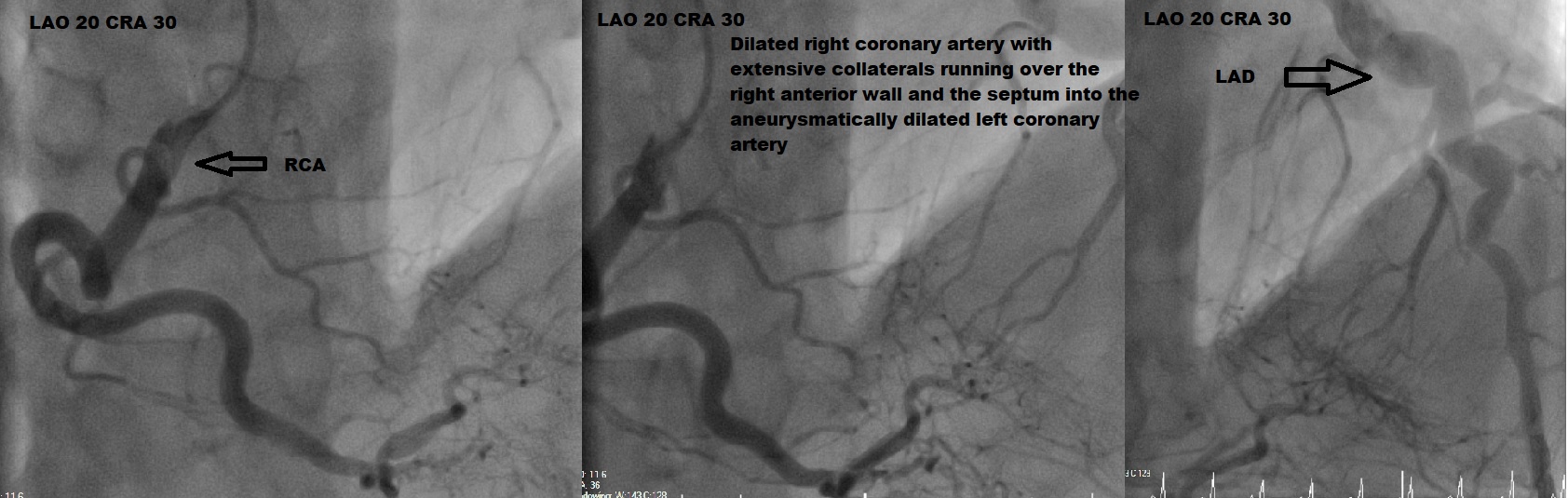
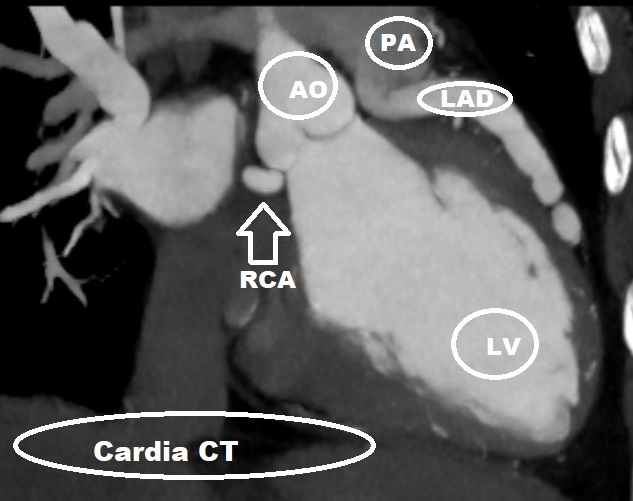
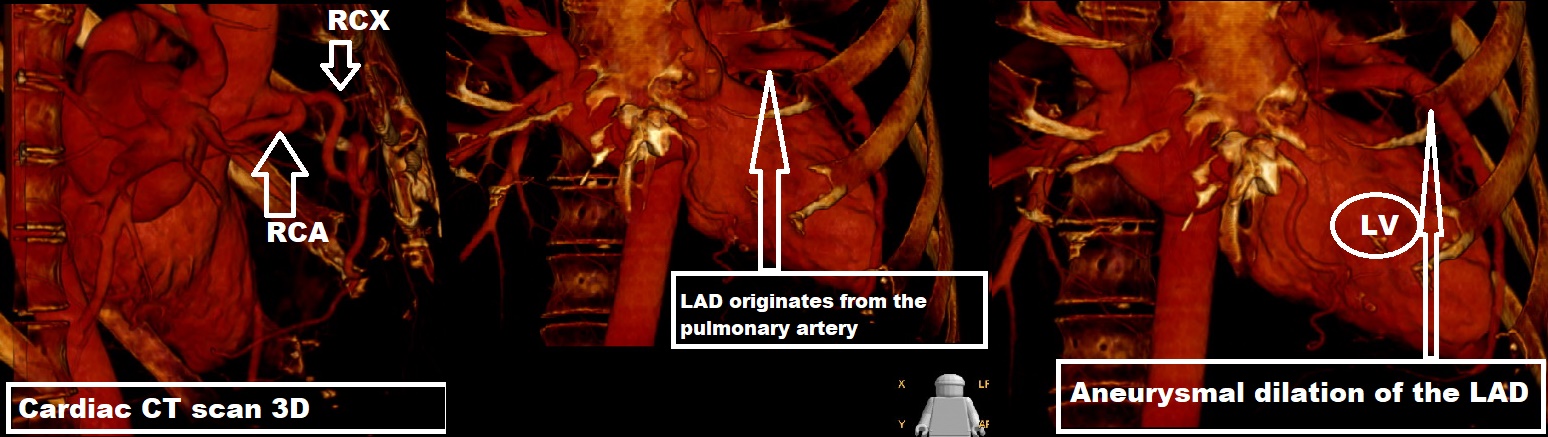
We report a case of a 52-year-old male who presented with progressive exertional dyspnea and clinical signs of heart failure. Electrocardiography showed no typical signs of ischemia. Laboratory findings showed significantly elevated N-terminal pro-B-type natriuretic peptide. Transthoracic echocardiography revealed severely impaired left ventricular ejection fraction. Coronary angiography was performed and showed a complex double coronary anomaly with an anomalous origin of the left coronary artery from the pulmonary artery with extensive collateralization from the right coronary artery supplying the left coronary system. Additionally, an anomalous origin of the circumflex artery from the right coronary artery with benign course, which is one of the most common coronary artery anomalies, was found. The diagnosis was subsequently confirmed by computed tomographic (CT) coronary angiogram with 3D reconstruction, which showed ectatic RCA arising from the right coronary sinus and the left descending artery arising from the pulmonary artery. Cardiac Magnetic Resonance (MR) demonstrated thinning of anterolateral wall of the left ventricle with sub endocardial delayed gadolinium enhancement.
MANAGEMENT AND CONCLUSION:
The patient was immediately started on guideline-directed medical therapy for heart failure, titrated to the maximum tolerated dose. Following a discussion in the multidisciplinary Heart Team, the patient was scheduled for definitive surgical correction to establish a dual coronary artery system and restore normal myocardial perfusion. This case highlights the importance of considering rare congenital anomalies in the differential diagnosis of ischemic dilated cardiomyopathy in adults, even in the fifth decade of life. Advanced imaging techniques like coronary angiography and cardiac CT are crucial for accurate diagnosis. Surgical revascularization remains the treatment of choice to prevent further myocardial damage, to prevent adverse outcome and improve long-term prognosis.