Background:Autonomic dysfunction may contribute to the development of atrial fibrillation detected after stroke (AFDAS), yet the clinical relevance of autonomic biomarkers remains unclear. This study investigated the association between cardiac autonomic function (CAF) assessed by periodic repolarization dynamics (PRD) and deceleration capacity (DC) and the risk of AFDAS.
Methods:Between February 2021, and May 2023, a total of 263 patients with acute ischemic stroke (AIS) from the STROKE-CARD II cohort who were hospitalized at the Medical University of Innsbruck were prospectively enrolled. All participants were in sinus rhythm at baseline and without a history of atrial fibrillation (AF). CAF was evaluated using 30-minute ECG recordings during hospitalization. PRD and DC were calculated using validated signal processing algorithms. AFDAS was assessed during a 12-month follow-up period via standardized cardiovascular evaluations. To assess baseline clinical risk, the CHASE-LESS score was calculated for each patient.
Results:The median age of the cohort was 67 years (IQR 16.5), and 31.2% were female. New-onset AF was identified in 25 patients (9.5%), who were significantly older than those without AF (median 75 vs. 66 years, p < 0.001). These patients also exhibited higher PRD values (median 5.80 vs. 2.93 deg², p = 0.005; Figure 1) and lower DC values (median 4.01 vs. 5.78 ms, p = 0.019; Figure 2). In multivariable logistic regression, pathologic PRD (≥5.75 deg²) independently predicted new-onset AF (odds ratio [OR] 2.47, 95% confidence interval [CI]: 1.01–6.02, p = 0.045), alongside age (OR per year 1.075, 95% CI: 1.03–1.13, p = 0.004). In contrast, pathological DC was not a significant predictor of new-onset AF in the adjusted model (OR 1.32, 95% CI: 0.49–3.55, p = 0.583). Gender was also not associated with new-onset AF (p = 0.999). The CHASE-LESS score alone showed moderate predictive accuracy (AUC = 0.67), which improved significantly when CAF parameter were added to the model (AUC = 0.81, p = 0.005).
Conclusions:Altered cardiac autonomic regulation, characterized by increased sympathetic and decreased parasympathetic activity, was significantly associated with AFDAS in our study. The addition of autonomic biomarkers to clinical risk scores like CHASE-LESS may improve AF risk stratification and guide individualized monitoring strategies after stroke.
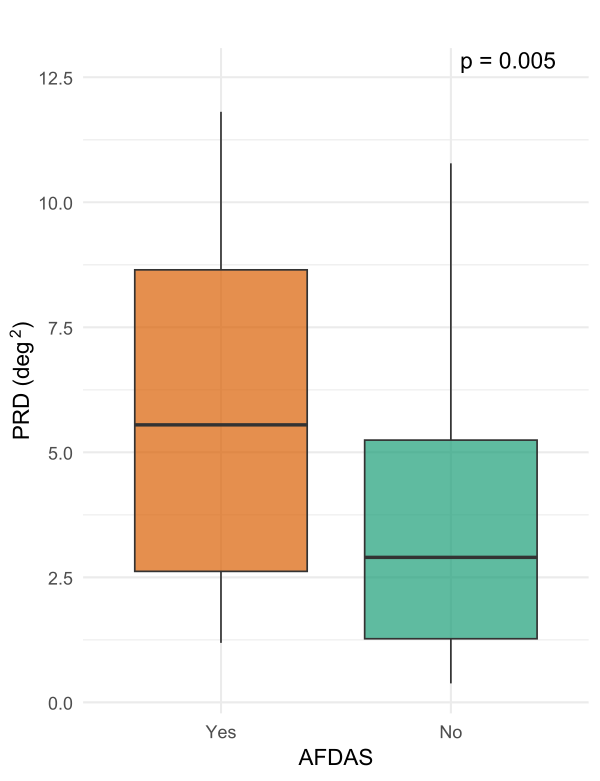
Figure 1: Comparison of periodic repolarization dynamics (PRD) between patients with and without atrial fibrillation detected after stroke (AFDAS) after stroke.
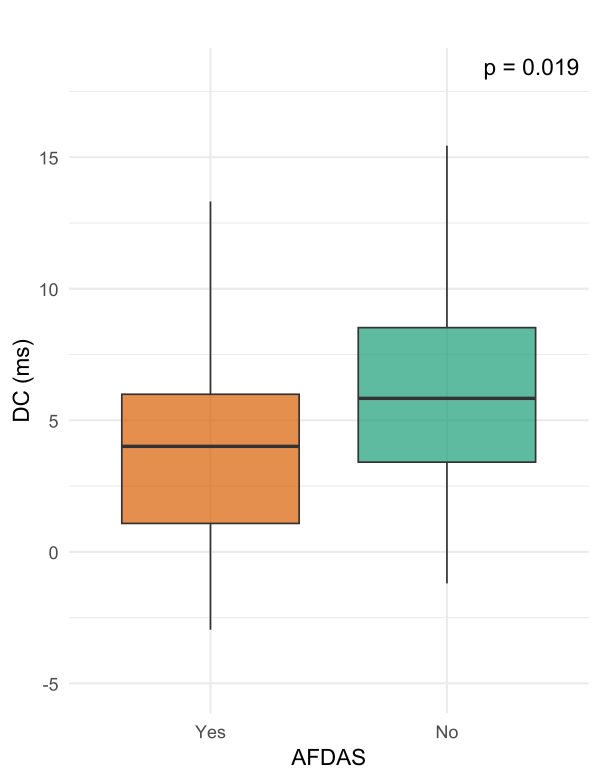
Figure 2: Deceleration capacity (DC) in patients with and without atrial fibrillation detected after stroke (AFDAS) following stroke.
