Background
Catheter ablation is a cornerstone in the management of atrial fibrillation (AF) in patients with heart failure with reduced ejection fraction (HFrEF). While thermal energy-based techniques such as cryoballoon ablation have been extensively studied, Pulsed Field Ablation (PFA) has recently emerged as a promising non-thermal alternative. Its performance in HFrEF patients, however, remains to be defined.
Objective
To compare clinical and procedural outcomes of PFA and cryoballoon ablation in HFrEF patients undergoing first-time pulmonary vein isolation (PVI).
Methods
We analyzed 93 consecutive HFrEF (LVEF ≤ 40%) patients who underwent PFA-based PVI between 2022 and 2025 and compared them with a historical cohort of HFrEF patients treated with cryoballoon PVI between 2012 and 2017 (Cryo1000 registry). The primary endpoint was recurrence of any atrial arrhythmia >30 seconds after a blanking period (BP) of 3 months. If a repeat procedure was performed during BP this was rated as an endpoint. Procedural metrics were also compared.
Results
A total of 25 PFA patients and 68 cryoballoon patients were included. Baseline characteristics were generally balanced, although the PFA group had a higher prevalence of male sex (79% vs 52%, p<0.05), persistent AF (70% vs 36%, p<0.01), and lower LVEF (31% vs 35%, p<0.05).
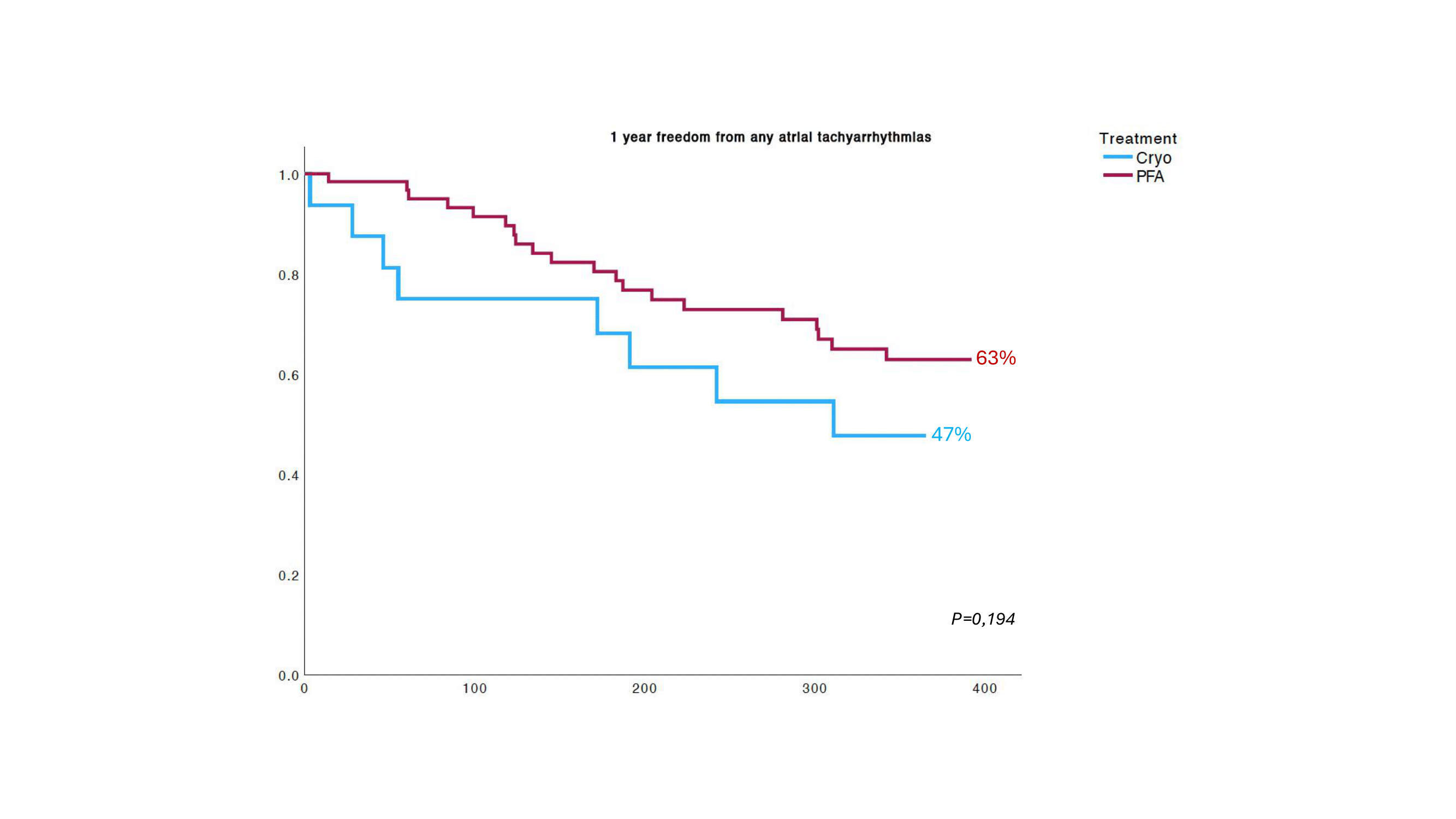
Procedural time was significantly shorter in the PFA group (34 vs 65 min, p<0.001), as was fluoroscopy time (7.3 vs 9.7 min, p<0.01). There were no major complications in both group and only one complication at access site occured in the PFA group. The PFA group showed a lower recurrence rate of atrial arrhythmias at 1 year (47% vs 63%, p= 0,194).
Conclusion
Both technologies showed a good safety profile. PFA demonstrated shorter procedural and fluoroscopy times and furthermore a trend toward lower arrhythmia recurrence rates at 1 year. These findings support rhythm control with PVI as first line strategy in this vulnerable patient cohort and a potential clinical benefit of PFA, which has to be confirmed in larger trials.