Background: Right ventricular (RV) dysfunction has been reported as an independent prognostic parameter in patients with cardiac amyloidosis (CA). The afterload-adjusted parameters of RV function may provide a more comprehensive insight into RV performance. This study aims to assess the prognostic value of echocardiographic surrogates of RV-pulmonary artery (PA) coupling in cardiac immunoglobulin light chain (AL) and transthyretin (ATTR) amyloidosis.
Methods: We retrospectively analyzed RV-PA coupling in consecutive patients with AL or ATTR-CA from our center diagnosed between 2014 and 2023. RV-PA coupling was assessed using three different echocardiographic surrogates: tricuspid annular plane systolic excursion/pulmonary artery systolic pressure (TAPSE/PASP), fractional area change/PASP (FAC/PASP), and RV free wall strain/PASP (RVFWS/PASP) ratios. Median values were determined to identify RV-PA uncoupling and stratify the population. The primary endpoint was all-cause mortality.
Results: 133 patients with CA (83% with ATTR-CA, 17% with AL-CA) were included in the study (median age 77 years, 87% male). During a median follow-up period of 23 months (IQR: 15-34) the primary endpoint of all-cause mortality occurred in 29 patients (22%). The median values of TAPSE/PASP, FAC/PASP, and RVFWS/PASP were 0.41 mm/mmHg (IQR: 0.32-0.60), 0.88 %/mmHg (IQR: 0.62-1.18), and 0.41 %/mmHg (IQR: 0.29-0.63), respectively. RV-PA uncoupling at the diagnosis of CA was observed in 52% of the study patients when using TAPSE/PASP and FAC/PASP, and 51% when using the RVFWS/PASP ratio. Patients exhibiting RV-PA uncoupling were older, more symptomatic, had worse systolic left ventricular (LV) and RV function as well as higher NT-proBNP levels and poorer laboratory parameters indicative of secondary organ damage (Table 1). Impaired RV-PA coupling was associated with an increased all-cause mortality as indicated by a TAPSE/PASP ratio <0.41 (hazard ratio (HR) 4.19, 95% confidence interval (CI) 2.02–8.69, p = 0.001; figure 1), and these findings remained consistent in both AL- and ATTR-CA patient cohorts. Receiver operating characteristic (ROC) analysis revealed that the TAPSE/PASP ratio exhibited the best predictive value for outcomes (area under the curve (AUC) = 0.700, 95% CI: 0.560–0.840) when compared to FAC/PASP (AUC = 0.676, 95% CI: 0.541–0.811) and RVFWS/PASP (AUC = 0.662, 95% CI: 0.532–0.793).
Conclusions: Early RV-PA uncoupling is linked to a higher risk of all-cause mortality in CA patients. TAPSE/PASP outperforms FAC/PASP and RVFWS/PASP in predicting long-term survival.
Table 1. Baseline characteristics of the study population stratified by RV-PA uncoupling (TAPSE/PASP <0.41 mm/mmHg)
| Variable |
All
N = 133 |
Impaired RV-PA coupling
N = 69 |
Normal RV-PA coupling
N = 64 |
P value |
| Age, years |
77 (72-81) |
79 (75-84) |
76 (72-80) |
0.008 |
| NYHA class ≥3, n (%) |
39 (29) |
26 (37) |
13 (21) |
0.048 |
| LVEF, % |
48 ± 11 |
44 ± 12 |
52 ± 9 |
<0.001 |
| LVGLS, % |
-11.8 ± 4.2 |
-10.4 ± 3.7 |
-13.1 ± 4.3 |
<0.001 |
| TAPSE, mm |
16 ± 5 |
13 ± 3 |
19 ± 4 |
<0.001 |
| FAC, % |
34 ± 10 |
29 ± 9 |
39 ± 8 |
<0.001 |
| RVFWS, % |
-16.0 ± 5.8 |
-12.6 ± 4.0 |
-19.6 ± 5.2 |
<0.001 |
| RVGLS, % |
-12.1 ± 4.7 |
-9.6 ± 3.1 |
-15 ± 4.5 |
<0.001 |
| NT-proBNP, ng/l |
2583 (1255-5728) |
5100 (2681-10279) |
1661 (729-3172) |
<0.001 |
| Creatinine, μmol/l |
108 (93-143) |
117 (99-159) |
101 (84-118) |
0.003 |
| Bilirubin, mg/dl |
12 (9-18) |
15 (10-25) |
11 (8-15)
|
0.005 |
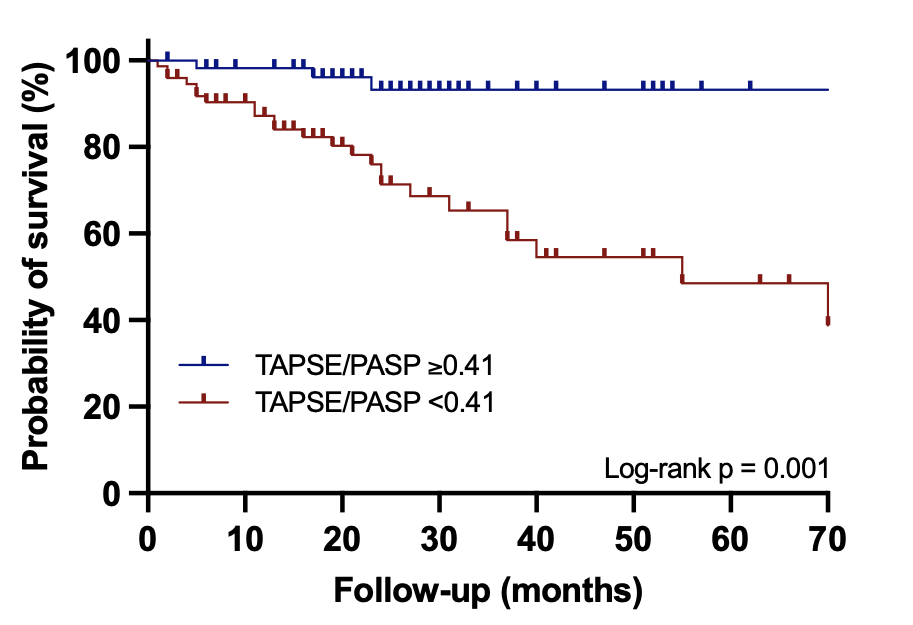
Figure 1. Kaplan-Meier survival analysis in CA patients with vs. without RV-PA uncoupling





