Introduction: Pre-hospital ECG at admission of patients with suspected acute coronary syndrome (ACS) is the most important tool in order to promptly identify patients with ST-elevation myocardial infarction (STEMI). However, the predictive value, as well as sex-specific differences of a pathologic pre-hospital ECG for identifying non-STEMI (NSTEMI) patients with type 1 myocardial infarction (MI) requiring percutaneous coronary intervention (PCI) remains controversial.
Purpose: To test sex-specific differences in the prognostic value of a pathologic pre-hospital ECG for identifying patients with NSTEMI requiring PCI.
Methods: Between 1/2014 and 11/2021 we retrospectively identified patients with available pre-hospital ECG, who underwent a coronary angiography due to suspected ACS at a single tertiary center (LMU-university hospital). Patients with STEMI were excluded from the analysis. A pathological (ischaemic) ECG was defined as the composite of ST-depression, ST-elevation not meeting the criteria for STEMI or T-wave inversion in at least one ECG lead, left bundle branch block (LBBB) or ventricular fibrillation (VF)/ventricular tachycardia (VT). The primary endpoint of the study was a target-lesion revascularization. The secondary endpoint was intrahospital mortality. The association between an ischaemic-ECG and the endpoints was tested using logistic-regression analysis adjusted for age. The effect of sex on the predictive value of an ischaemic-ECG for identifying patients with NSTEMI requiring PCI was estimated using interaction-analysis.
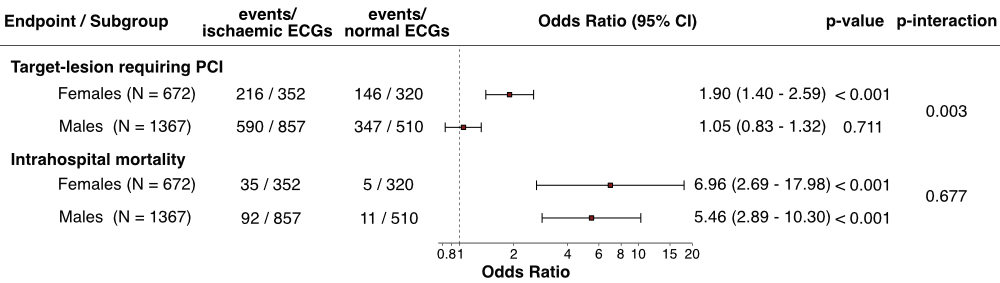
Results: We identified 2.039 patients (672 females; 33%) with available pre-hospital ECG recordings, who underwent a diagnostic coronary angiography due to suspected ACS. The mean age of the patients was 67 ± 18 years. In 1.299 (64%) cases a successful PCI was performed. An ischaemic ECG was present in 1.209 (59%) patients. Males presented with an ischaemic ECG (63%) more frequently than females (52%; p < 0.001), primarily driven by a higher-rate of VF and VT (Table 1). Moreover, male sex was more frequently associated with the primary endpoint, than female sex (69% vs. 54%; p < 0.001). An ischaemic ECG was highly prognostic for death in both females (OR 6.96; 95% CI 2.69 – 17.98; p < 0.001) and males (OR 5.46; 95% CI 2.89 – 10.30; p < 0.001; p-interaction = 0.677; Figure 2). However, an ischaemic ECG was associated with target-lesion revascularization only in female (OR 1.90; 95% CI 1.40 – 2.59; p <0.001), but not in male patients (OR 1.05; 95% CI 0.83 – 1.32; p = 0.711; p-interaction = 0.003; Figure 2).
Conclusion: Ischaemic ECG changes are associated with a 6-fold mortality in male and female patients undergoing diagnostic coronary angiography because of suspected ACS. Male patients present with ischaemic pre-hospital ECG more frequently. Although male sex is associated with target-lesion revascularization, an ischaemic ECG was not associated with target-lesion revascularization in males but only in females.
|
Parameter
|
Males
|
Females
|
p-value
|
|
N (%)
|
1367 (67%)
|
672 (33%)
|
|
|
Age, years ± SD
|
66 ± 18
|
70 ± 18
|
< 0.001
|
|
Ischaemic ECG
· ST-depression
· ST-elevation not meeting STEMI criteria
· T-wave inversion
· LBBB
· VF
· VT
|
857 (63%)
328 (24%)
408 (30%)
479 (35%)
61 (4%)
63 (5%)
36 (3%)
|
352 (52%)
180 (27%)
177 (26%)
217 (32%)
45 (7%)
11 (2%)
7 (1%)
|
< 0.001*
0.266*
0.136*
0.123*
0.072*
0.002*
0.029*
|
|
Target lesion requiring PCI
|
937 (69%)
|
362 (54%)
|
< 0.001*
|
|
Intrahospital mortality
|
103 (8%)
|
40 (6%)
|
0.192*
|