Background
Arterial stiffness (AS) is currently under evaluation as a marker of cardiovascular diseases. AS can be assessed non-invasively as aortic pulse wave velocity (PWV) and aortic distensibility (AD) by cardiovascular magnetic resonance (CMR) imaging.
Methods
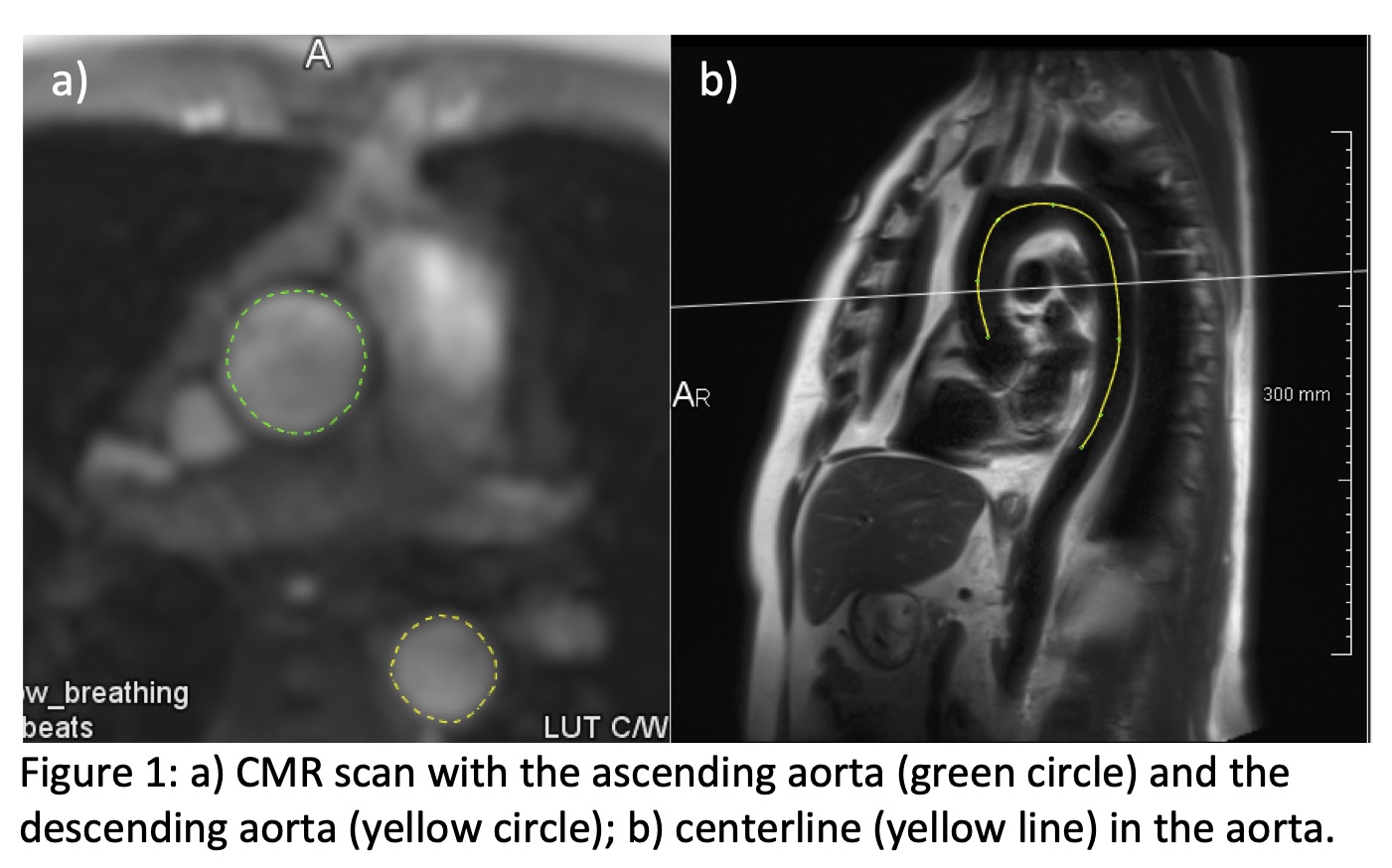
This analysis was based on the first 10,000 participants of the Hamburg City Health Study (HCHS). All CMR scans for AS analysis were performed at a 3T magnetic resonance imaging (MRI) scanner (MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany). PWV and AD are quantified based on blood flow measurements in 2D phase-contrast MRI (PC-MRI) data and the centerline of the aorta in black-blood sequences (Figure 1). PWV was quantified using the 50% method and AD was quantified using the formula according to Harloff et al., 2009, in the ascending (AD AoAsc) and descending aorta (AD AoDesc). All CMR scans were analyzed by two blinded observers.
Results and perspective
2,270 participants underwent a CMR scan. The median age of this CMR cohort was 66.50 [59.00, 72.00] and 942 (41.50%) participants were female. Intraclass correlation coefficients (ICCs) between different observers were 0.99 [0.99-0.99] for PWV, 0.97 [0.97-0.97] for AD AoAsc and 0.99 [0.99-0.99] for AD AoDesc. PWV, AD AoAsc and AD AoDesc were 5.80 [4.91, 7.19] m/s, 0.54 [0.34, 0.78] 1/(10^3*kPa) and 0.61 [0.39, 0.84] 1/(10^3*kPa) in healthy individuals without any cardiovascular risk factor (CVRF) and/or CV disease and 7.85 [6.33, 9.93] m/s, 0.38 [0.25, 0.59] 1/(10^3*kPa) and 0.41 [0.27, 0.61] 1/(10^3*kPa) in participants with at least one CVRF and/or CV disease (all p<0.001). Significant associations of PWV were found with hyperlipidemia (p<0.001, r=0.0073), atrial fibrillation (p<0.001, r=0.0286) and hypertension (p<0.001, r=0.1190); but also with smoking (p=0.003, r=0.0050) and a history of myocardial infarction (p=0.012, r=0.0164). AD AoAsc was significantly associated with atrial fibrillation (p<0.001, r=0.0885), hypertension (p<0.001, r=0.0553) and diabetes (p=0.016, r=0.0163). AD AoDesc was significantly associated with hypertension (p<0.001, r=0.0641) and BMI (p=0.043, r=0.0034).
Conclusion
PWV and AD can be quantified by CMR 2D PC-MRI with an excellent inter-observer agreement. Higher PWV and lower AD are significantly associated with cardiovascular risk factors and diseases, in particular with hypertension.