Background
Catheter ablation of atrial fibrillation (AF) aiming at pulmonary vein isolation (PVI) is a time-demanding procedure. Ablation settings using high power and short energy (HPSD) application have been introduced into clinical practice. Modern mapping catheters allow for high-density mapping during ablation procedures. We systematically assessed the implementation of high-density mapping catheters and HPSD ablation protocols into our institutional routine workflow and its impact on procedural timings, efficacy and safety.
Methods
Three ablation setups for PVI were analyzed: 1) Ablation under guidance of a lesion quality index (Ablation index=AI) (30/35W AI) alongside mapping with a circular catheter; 2) HPSD using 50 W under AI-guidance and mapping with a pentaspline mapping catheter (50W AI); 3) HPSD ablation with 90W over 4 seconds with a novel catheter allowing for high energy setting ablation and mapping with a pentaspline catheter (90W/4-sec group). Lab cycle analysis was performed on 6 procedural steps (Preprocedural preparation, vascular access and transseptal puncture, left atrial mapping, ablation, validation of PVI and vascular closure, post-procedural preparation) using a specific computer application (Lab Optimization Tool, Biosense Webster). Total procedure times as well as “skin-to-skin” times from vascular access to closure were assessed. Follow-up included clinical investigation, TTE, ECG and Holter ECG (24-72 hours after 6 and 12 months and every 6 to 12 months afterwards.
Results
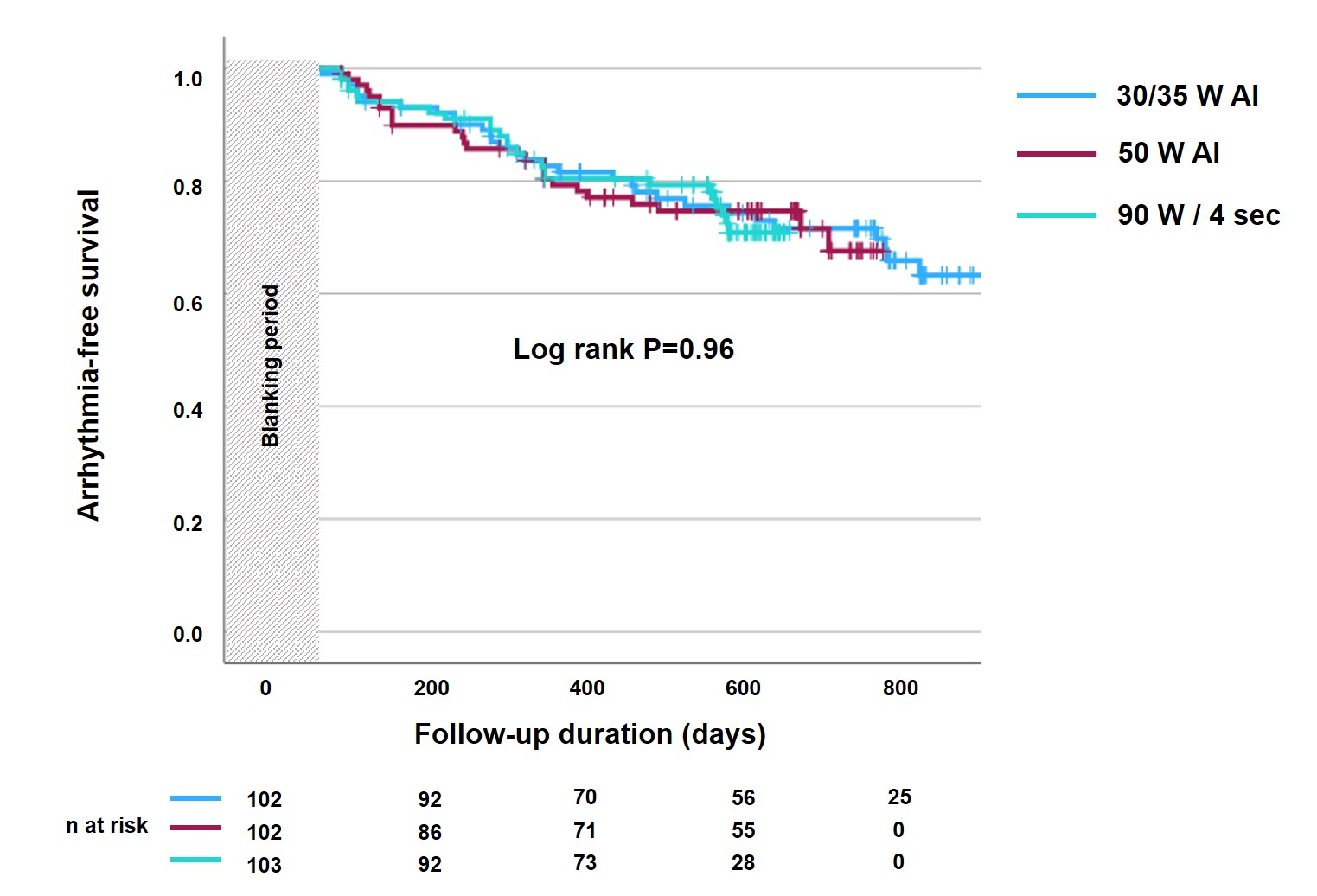
A total of 307 patients were analyzed (30/35W AI n=102, 50W AI n=102, 90W/4 sec n=103). Patients baseline data are shown in Table 1. Skin-to-skin times (105.3±22.7 minutes (30/35W AI) vs. 81.4±21.3 minutes (50W AI) vs 69.5±12.2 minutes (90W/4 sec), P=<0.001) and total laboratory times (132.8±42.1 minutes vs. 107.4±25.7 minutes vs 95.2±14.0 minutes, p<0.001) were significantly different among study groups (Figure 1, Table 2). Laboratory interval analysis showed shortened mapping and ablation times resulted in above mentioned differences (Figure 1, Table 2). Arrhythmia-free survival after 12 months was not significantly different among study groups (log rank P=0.96) (Figure 2).
Conclusion
The incorporation of high-density mapping and HPSD into AF ablation led to procedural time shortening durations without compromising effectiveness and safety in AF ablation.
Table 1
|
Parameter
|
35/30 W
|
50 W
|
90 W
|
P value
|
|
Patients, n
|
102
|
102
|
103
|
|
|
Female, n (%)
|
35 (34.3)
|
32 (31.4)
|
32 (31.1)
|
0.86
|
|
Age (years)
|
67.7±11.4
|
65.4±11.2
|
66.9±10.4
|
0.32
|
|
LA diameter (mm)
|
45.6±3.3
|
46.1±3.1
|
45.5±4.2
|
0.44
|
|
LVEF (%)
|
51.1±9.7
|
50.9±10.2
|
52.1±7.7
|
0.61
|
|
Paroxysmal AF, n (%)
|
37 (36.3)
|
35 (34.3)
|
34 (33.0)
|
0.89
|
|
Persistent AF, n(%)
|
67 (65.7)
|
70 (68.6)
|
69 (67.0)
|
0.90
|
|
CHA2DS2-VASC-Score, median (IQR)
|
2 (2;4)
|
3 (2;4)
|
2 (1;3)
|
0.92
|
Data are presented as n (%) or mean±standard deviation.
Table 2
|
Parameter
|
Pre-procedural [min]
|
Vascular access + TSP [min]
|
Mapping [min]
|
Ablation [min]
|
Validation + vascular closure [min]
|
Post-procedural [min]
|
“Skin-to-skin“ [min]
|
Total duration [min]
|
|
30/35W AI-guided
|
20.7±7.1
|
30.2±10.7
|
19.3±5.7
|
51.1±14.1
|
4.7±2.4
|
6.8±3.0
|
105.3±22.7
|
132.8±42.1
|
|
50W AI-guided
|
19.1±6.6
|
28.5±12.7
|
15.2±5.2
|
34.2±11.8
|
3.5±1.8
|
6.9±2.1
|
81.4±21.3
|
107.4±25.7
|
|
90W / 4 sec
|
19.0±5.9
|
27.7±10.2
|
13.1±6.9
|
25.4±8.9
|
3.3±2.1
|
6.7±1.7
|
69.5±12.2
|
95.2±14.0
|
|
P value
|
0.11
|
0.27
|
<0.001
|
<0.001
|
<0.001
|
0.83
|
<0.001
|
<0.001
|
Data are presented as mean±SD.
Figure 1
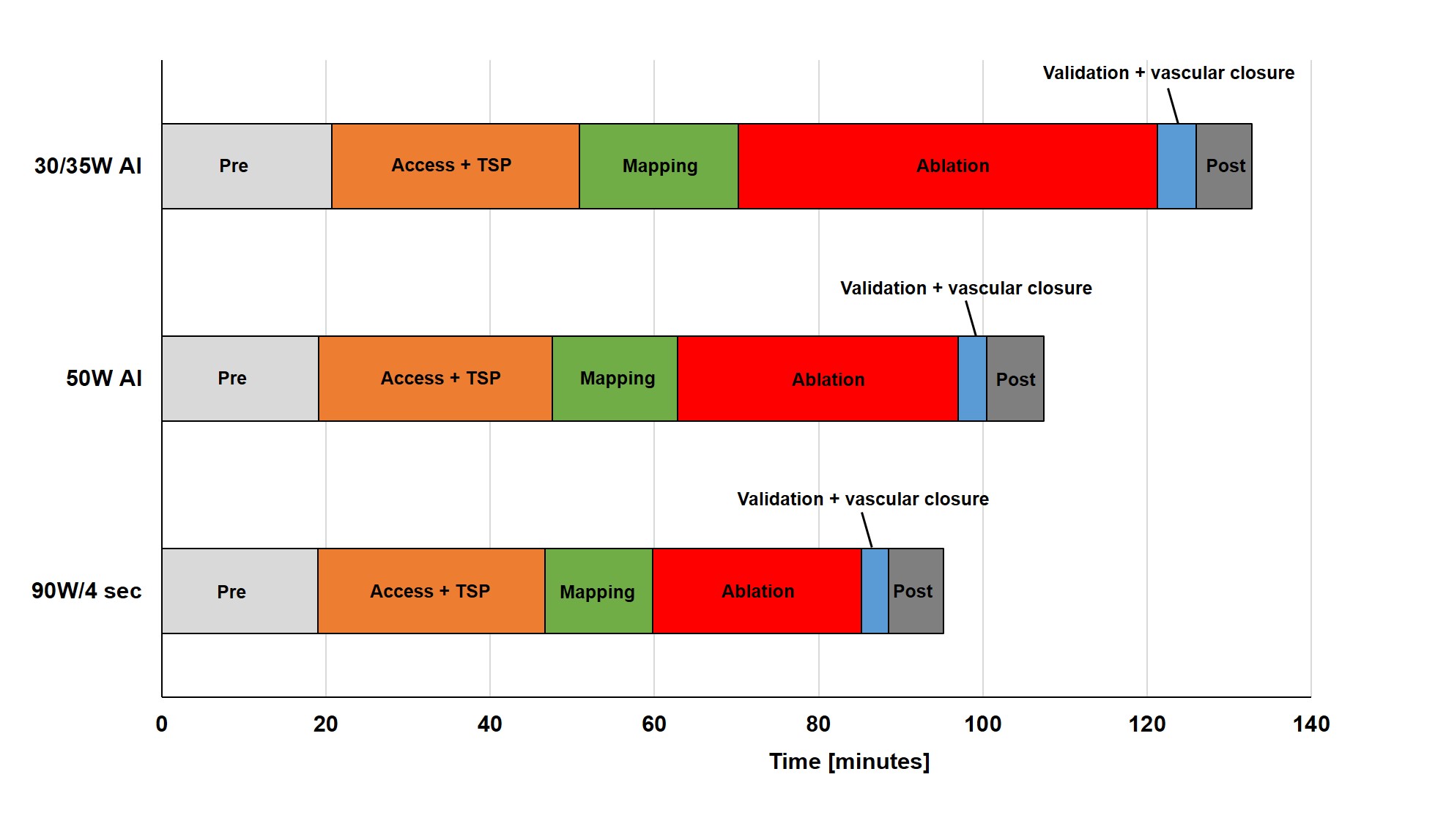 Figure 2
Figure 2