Background: Despite advances in mapping and ablation techniques, atrial fibrillation (AF) recurrence remains a challenge after pulmonary vein isolation. Low voltage areas (LVA) in the left atrium are associated with higher recurrence rates after left atrial ablation. Risk scores for evaluating post-ablation recurrences are not well established, although a better patient selection for repeat procedures would be of great help in clinical practice.
Methods: This single-center study includes consecutive patients from the prospective Bernau ablation registry undergoing ultra-high-density (UHD) mapping and repeat ablation for AF/AT recurrence between 2016 and 2020. The potential of seven guideline mentioned risk scores (APPLE, DR-FLASH, MB-LATER, ATLAS, CAAP-AF, BASE-AF 2, ALARMEc) to predict (1) AF/AT recurrence beyond a three-months blanking period after repeat left atrial ablation (Re-PVI ± further LA ablation) and (2) the percentage of left atrial LVA in UHD mapping was investigated. LVA were defined as sites with a bipolar peak-to-peak voltage of <0.5 mV with an extent of >1cm². Optimal cutoff for sensitivity and specificity for LVA and AF/AT recurrence as endpoint was chosen using C statistics with receiver-operator characteristics (ROC). Further ROCs were performed to illustrate the predictive ability of the scores. Pearson correlation was used to test associations between variables.
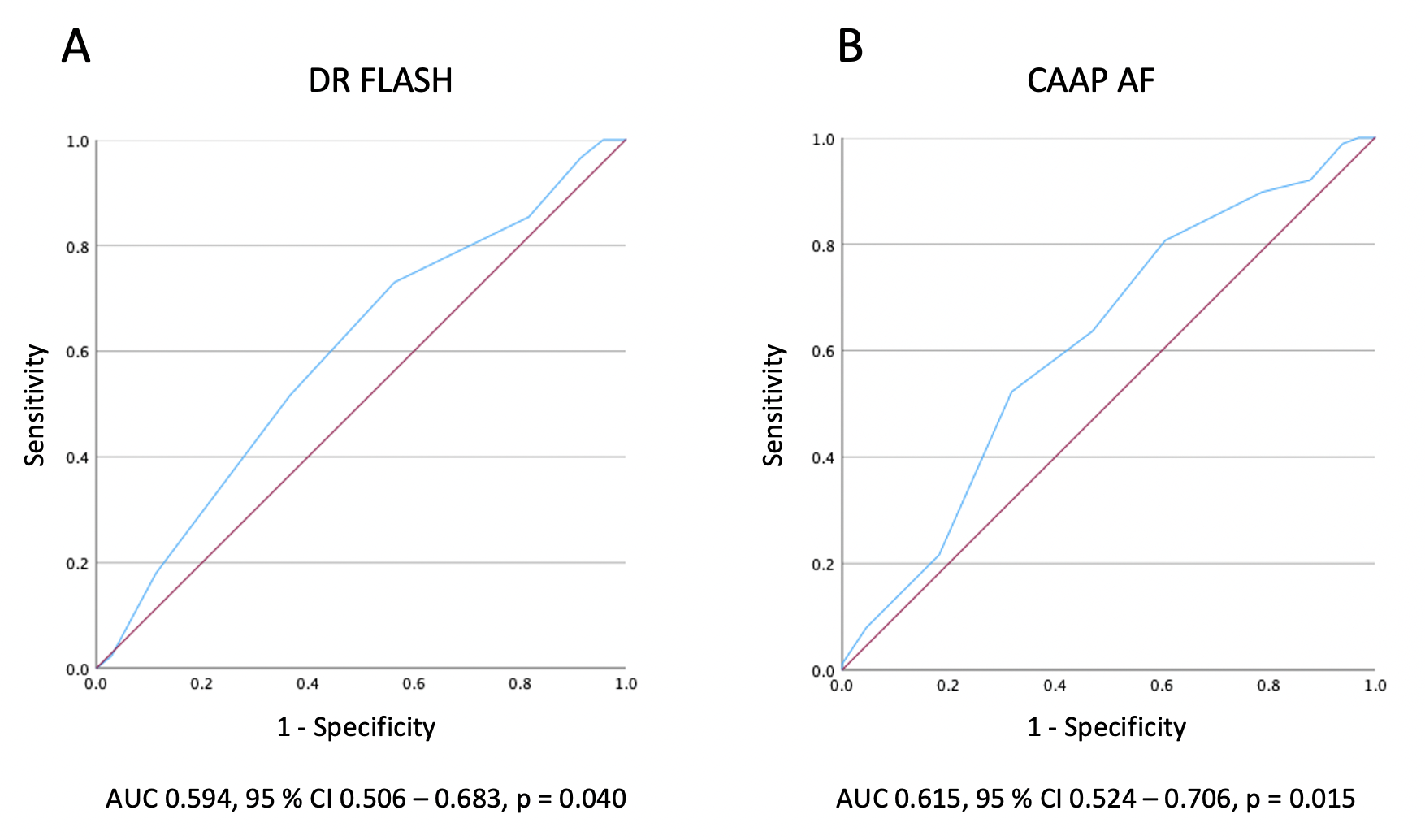
Results: 160 patients (mean age 67.9 ± 9.1 years, 60.6% persistent AF, mean AF duration 4.6 ± 3.8 years) with complete left atrial UHD mappings (mean EGMs 9754 ± 5808) were included. Baseline characteristics are presented in table 1. Overall recurrence rate over a mean follow-up time of 16 ± 11 months was 55.6%. The predictive value of the investigated risk scores on AF/AT recurrence in our cohort was low (Figure 1), with the highest power for CAAP-AF (p = 0.015, AUC = 0.615) and DR-FLASH score (p = 0.040, AUC = 0.594), Fig. 2. With respect to left atrial LVA we found a better predictive power for the CAAP-AF (p < 0.001, AUC 0.702), APPLE (p < 0.001, AUC 0.687), DR-FLASH (p < 0.001, AUC 0.688), ATLAS (p = 0.005, AUC 0.634) and ALARMEc (p = 0.007, AUC 0.608) score to predict low voltage based on a calculated cut-off of 22% of total left atrial surface (Fig. 1).
Conclusion: The predictive value of guideline-referred risk scores in estimating AF/AT recurrence after repeat ablation is low and does not seem to be of relevant help in patient selection for further interventional treatment. Some scores demonstrate a fairly good prediction for the amount of left atrial LVA and therefore might help in choosing the right mapping and ablation regime beforehand.
Table 1
|
|
Overall
n = 160
|
No recurrence
n = 71
|
Recurrence
n = 89
|
P-value
|
|
Age
|
67.9 (9.1)
|
67.0 (9.2)
|
68.5 (9.1)
|
0.285
|
|
Sex male (%)
|
81 (50.6)
|
42 (59.2)
|
39 (43.8)
|
0.054
|
|
BMI [kg/m2]
|
28.5 ± 5.0
|
28.1 ± 5.2
|
28.9 ± 4.9
|
0.334
|
|
CHA2DS2VASc-Score
|
3 IQR 3
|
3 IQR 3
|
3 IQR 2
|
0.116
|
|
AF duration [years]
|
4.6 ± 3.8
|
5.2 ± 4.9
|
4.2 ± 2.5
|
0.115
|
|
Atrial fibrillation (%)
|
142 (88.8)
|
66 (92.9)
|
76 (85.4)
|
0.105
|
|
paroxysmal
|
41 (25.6)
|
21 (29.6)
|
20 (22.5)
|
|
|
persistend
|
97 (60.6)
|
45 (63.4)
|
52 (58.4)
|
|
|
Atrial tachycardia (%)
|
18 (11.3)
|
5 (7.0)
|
13 (14.6)
|
|
|
Previous ablations [n]
|
1.3 ± 0.7
|
1.3 ± 0.5
|
1.4 ± 0.9
|
0.277
|
|
LVEF [%]
|
57.2 ± 6.9
|
57.9 ± 6.1
|
56.6 ± 7.5
|
0.239
|
|
NT-proBNP [pg/ml]
|
933 ± 1,434
|
859 ± 1,485
|
994 ± 1,397
|
0.560
|
|
Low voltage (<0.5 mV) area [%]
|
30.6 ± 23.1
|
18.8 ± 17.7
|
40.0 ± 22.6
|
<0.001
|
|
EGM points [number]
|
9,754 ± 5,808
|
8,722 ± 5,643
|
10,578 ± 5,838
|
0.044
|