Background:
Single-shot pulmonary vein isolation (ssPVI) using cryoablation (CBA) and pulsed field ablation (PFA) is an effective and safe therapeutic approach for patients (pts) with atrial fibrillation (AF). Preprocedural imaging (preIMG) with cardiac computed tomography (CT) or magnetic resonance imaging (MRI) is routinely used to assess the pulmonary vein (PV) anatomy before ablation. In this study, we evaluated the effects of preIMG on the procedural parameters, safety and effectiveness of ssPVI.
Methods:
Retrospective analysis of all AF patients who underwent their index ssPVI using the POLARx™ Cryoablation System or the FARAWAVE™ PFA system (Boston Scientific, MA, USA) in our center from 01.01.2022 to 15.12.2023. Preprocedural imaging data and the procedural parameters were analyzed. Major complications were defined as death, stroke or transient ischemic attack (TIA), atrial-esophageal fistula, cardiac tamponade and vascular access complications requiring surgical intervention. All patients were scheduled for follow-up visits six months after ablation. The Mann-Whitney U-test, the Fisher's exact test, the log-rank test and multivariate Cox regression models were performed using SPSS.
Results:
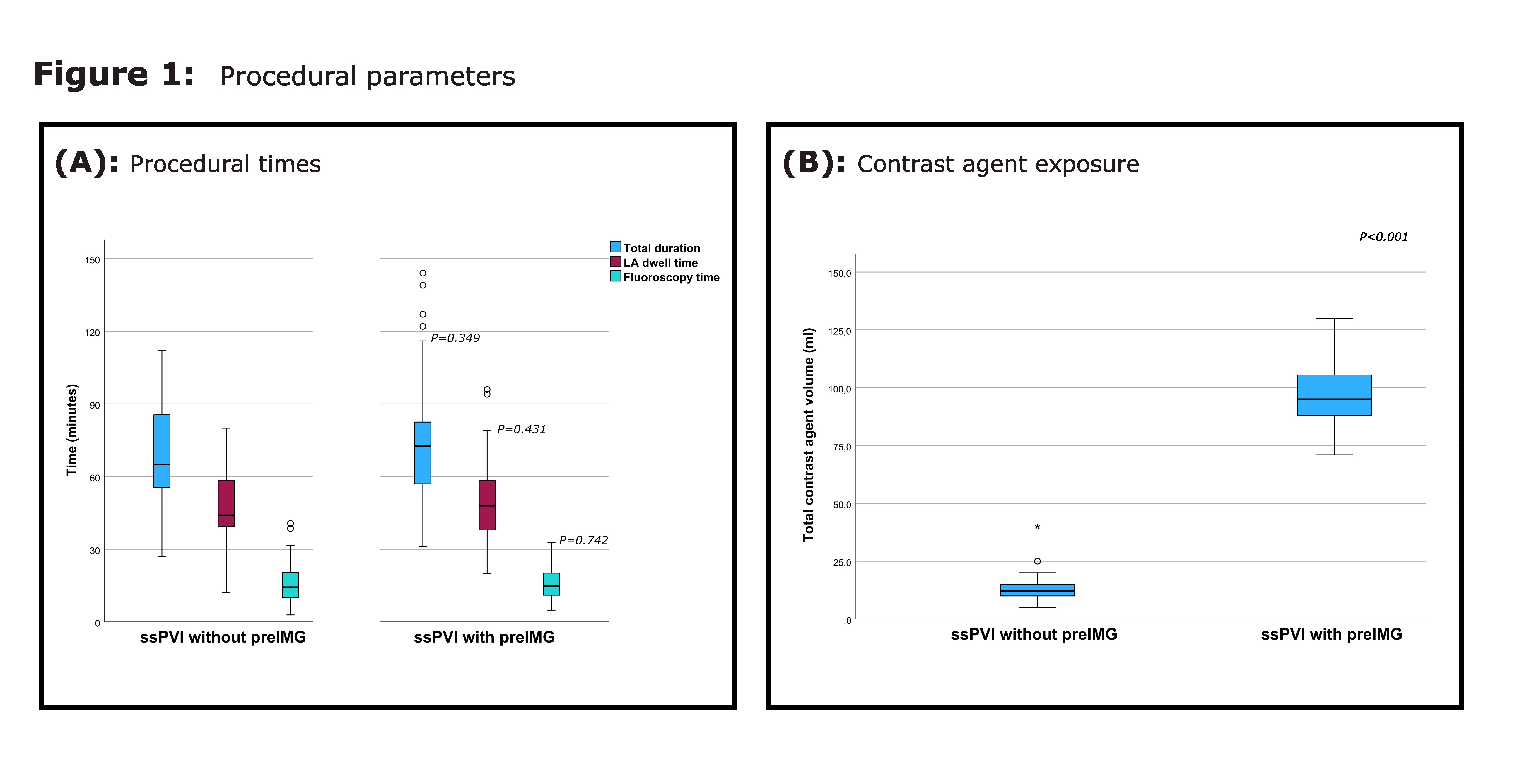
A total of 197 pts was enrolled (113 CBA and 84 PFA), thereof 132 pts received preIMG (117 CTs and 15 MRIs) and 65 patients received no preIMG before ssPVI. Baseline characteristics are summarized in Table 1. Both groups showed similar procedural performance(Figure 1). Two major complications occurred in the preIMG group (TIA and pseudoaneurysm of the femoral artery) while no major complications were observed in patients who did not receive preIMG (p=1). Pts who underwent preIMG were exposed to significantly higher amounts of contrast media (medians 95 vs. 12 ml, p<0.001) and had higher radiation exposure (median CT dose length product: 116 mGy.cm). Atypical PV anatomy was present in 32 pts (24%), whereas incidental findings requiring urgent investigation or therapy were present in 24 pts (18%)(Figure 2). Pts who did not undergo preIMG had comparable mid-term AF recurrence rate after 6 months (8% vs. 11% in the preIMG group, p=0.599). Multivariate analysis revealed that the ablation method (p=0.269) and the clinical AF type (p=0.401) did not have a significant influence on the risk of AF recurrence in our cohort (Figure 3).
Conclusions:
In this single-center retrospective study, the omission of preIMG was associated with significantly lower radiation dose and contrast media usage, while the procedural performance, safety profile and mid-term effectiveness were comparable to standard ssPVI with preIMG. Procedural guiding using fluoroscopy and intraprocedural selective angiography of the PV may be safe and sufficient to achieve PVI using modern single-shot approaches.
Table 1: Baseline Characteristics:
|
|
PVI with Pre- Imaging
|
PVI without Pre-Imaging
|
p-value
|
|
N
|
132
|
65
|
|
|
Age (mean ± SD, years)
|
66 ± 11
|
68 ± 10
|
0,128
|
|
AF type:
|
|
|
0,033
|
|
- Paroxysmal AF (%)
|
70 (53)
|
24 (37)
|
|
|
- Persistent AF (%)
|
62 (47)
|
41 (63)
|
|
|
Gender:
|
|
|
0,856
|
|
- Female (%)
|
47 (36)
|
24 (37)
|
|
|
- Male (%)
|
85 (64)
|
41 (63)
|
|
|
BMI median (IQR) (kg/m2)
|
29 (25 – 32)
|
28 (25 – 32)
|
0,657
|
|
Medical history
|
|
|
|
|
- CHF (%)
|
42 (32)
|
20 (31)
|
0,855
|
|
- CAD (%)
|
29 (22)
|
19 (29)
|
0,277
|
|
- HTN (%)
|
97 (74)
|
50 (77)
|
0,602
|
|
- DM (%)
|
26 (20)
|
12 (18)
|
0,836
|
|
- Stroke or TIA (%)
|
11 (8)
|
1(2)
|
0,061
|
|
- CHA2DS2-VASc-Score median (IQR)
|
3 (2 – 4)
|
3 (2 – 4)
|
0,449
|
|
Medication history
|
|
|
|
|
- Betablockers (%)
|
107
|
45
|
0,063
|
|
- Antiarrhythmic drugs (%)
|
24
|
11
|
0,828
|