Background
Transcatheter aortic valve implantation (TAVR) has established as the treatment of choice for high-risk patients with severe aortic stenosis (AS). Tricuspid regurgitation (TR) is often linked to AS and consecutive left-sided heart failure and is associated with adverse outcomes. Risk stratification through clinical scoring systems is vital for guiding therapeutic decisions.
Objectives
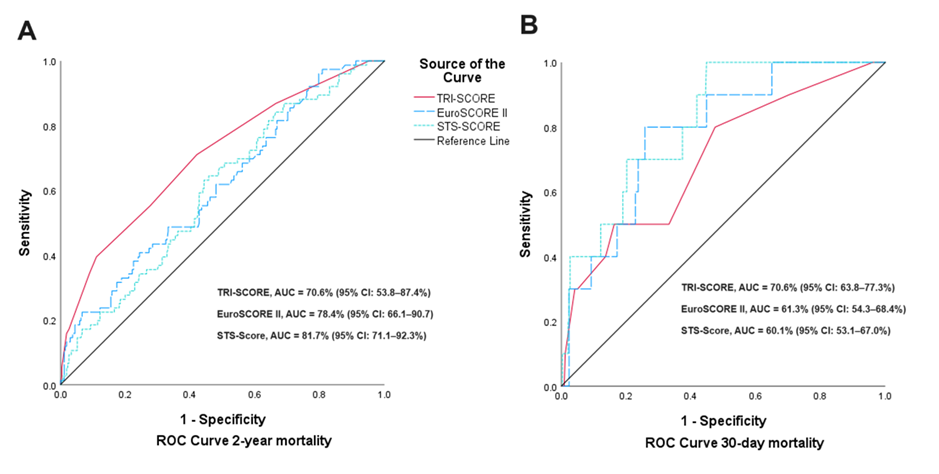
To assess the applicability of the TRI-SCORE for predicting adverse outcomes in patients with AS and concomitant moderate-to-severe TR undergoing TAVR and to compare its performance with established surgical rusk scores like the EuroSCORE II and Society of Thoracic Surgeons (STS) score.
Methods
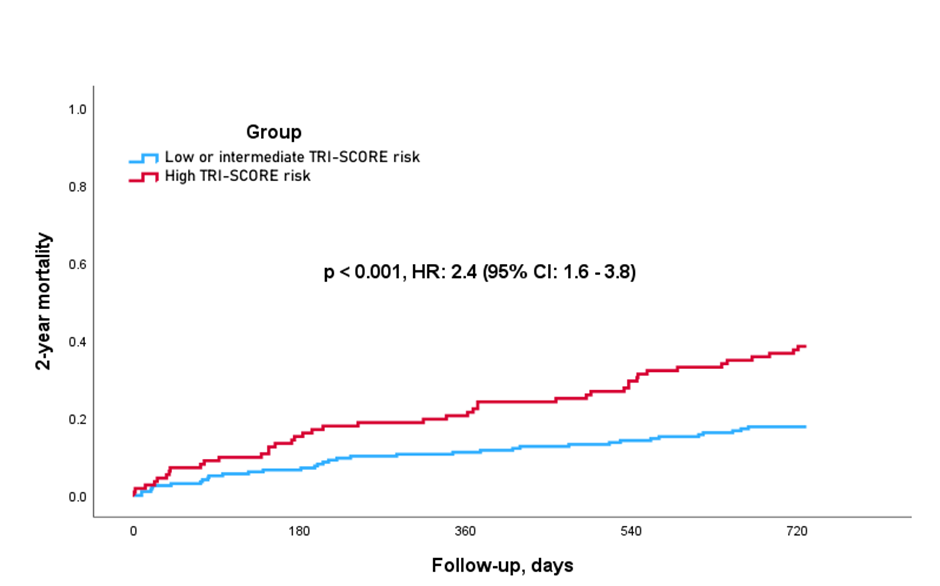
We conducted a retrospective analysis of 310 patients with severe AS and concomitant TR who underwent TAVR between 2013 and 2022 at the Heart Center Bonn. According to the TRI-SCORE, patients were stratified into a low or intermediate risk group (TRI-SCORE 0–5) and a high-risk group (TRI-SCORE 6–12). The primary endpoint was 2-year all-cause mortality. Predictive values of the TRI-SCORE were compared to the EuroSCORE II and the STS scores for both 30-day and 2-year mortality outcomes.
Results
The 2-year mortality rate was significantly higher in the high-risk group compared to the low or intermediate-risk group (38.4% vs. 17.7%; p < 0.001). For predicting 30-day mortality, the EuroSCORE II and the STS score demonstrated superior predictive values, with AUCs of 78.4% and 81.7%, respectively, in comparison to the TRI-SCORE, which showed an AUC of 70.6%. Conversely, the TRI-SCORE allowed a better risk prediction with regard to the 2-year all-cause mortality, achieving an AUC of 70.6%, superior to the EuroSCORE II (61.3%) and the STS Score (60.1%).
Conclusion
The TRI-SCORE is effective in predicting mid-term mortality in patients with AS and moderate-to-severe TR undergoing TAVR, demonstrating greater robustness than the EuroSCORE II and the STS score for this timeframe. While the AUC for the TRI-SCORE is acceptable, further refinement is necessary to enhance its predictive capabilities.