Background
Atrial cardiomyopathy (AtCM) is linked to new-onset atrial fibrillation (AF), heart failure, and a possibly increased risk of cardio-embolic stroke. Improving early detection of AtCM could therefore enhance treatment strategies, potentially preventing adverse clinical outcomes. AtCM is associated with electrical conduction slowing, which can be non-invasively quantified by a prolonged P-wave in the electrocardiogram (ECG). However, the late components of prolonged P-waves often have small amplitude and are easily missed by standard ECG delineation algorithms. Our group showed that precise measurement of the P-wave by experts after amplification of the digital ECG (sweep speed 150-200 mm/s, amplification 80 mm/mV) can diagnose and stage AtCM with high sensitivity and specificity.
Purpose
We hypothesize that standard ECG delineation algorithms systematically underestimate P-wave duration compared to amplified P-wave duration (APWD) due to low-amplitude segments, especially in more extensive AtCM stages, not being considered by standard algorithms.
Methods
To assess differences in P-wave duration between standard algorithms and APWD, ECGs of 3,420 participants from the Hamburg City Health Study (HCHS), a large, prospective, population-based cohort, were analysed. P-wave duration was assessed using two methods: first, the open source ECGDeli algorithm, which has been validated against other established P-wave delineation algorithms; second, manual APWD annotations by experts. Distributions of both measurements and their deviations were investigated and differences were analysed in relation to known cardiovascular risk factors for AtCM: age, sex, BMI, and CHA₂DS₂-VASc score.
Results
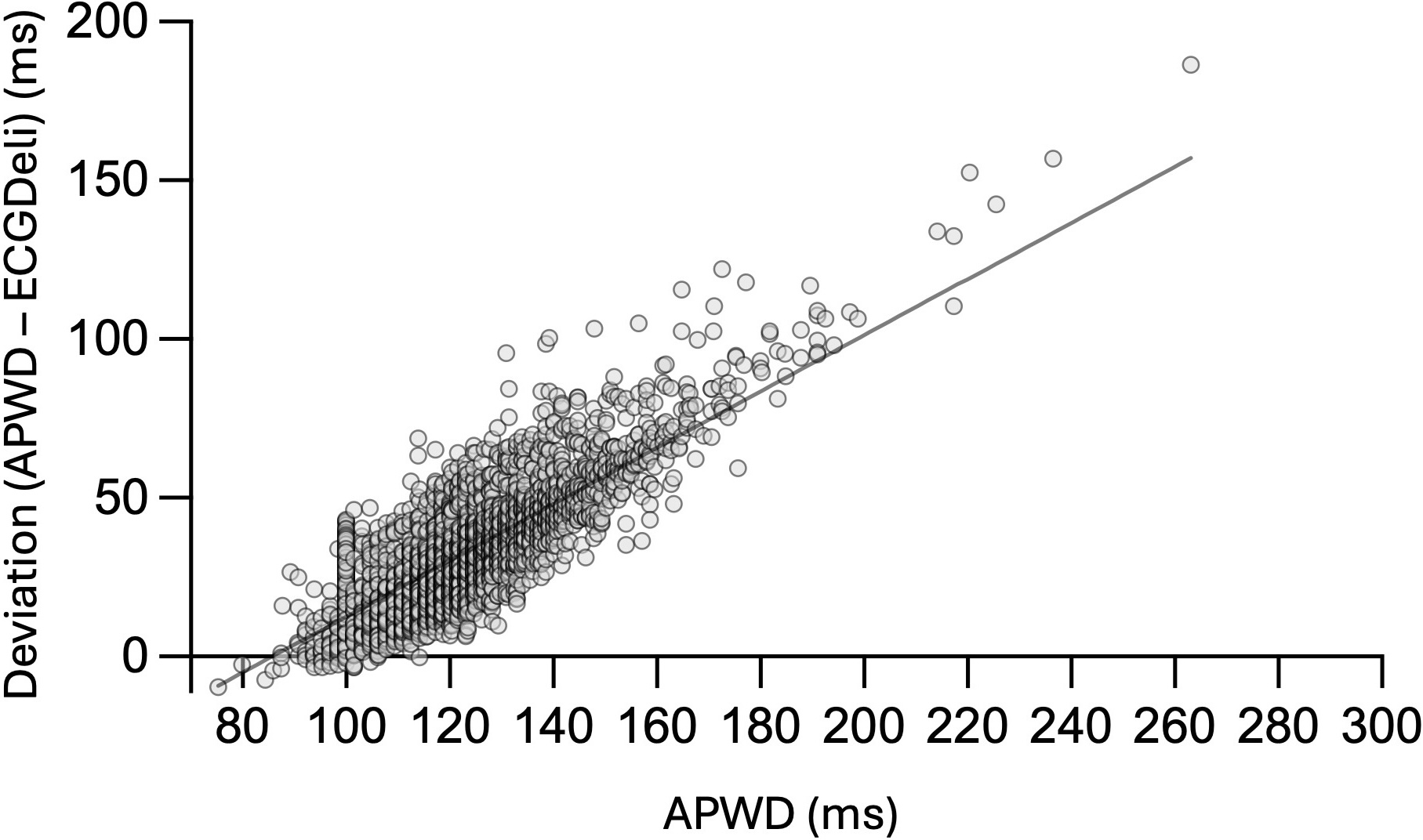
The mean of manually annotated APWD was 122 ± 17 ms, compared to ECGDeli’s 90 ± 12 ms. The maximum value measured with ECGDeli was 121 ms, close to the mean APWD annotation. The difference between the two methods correlated strongly with APWD (p< 0.001), with a greater difference for greater APWD. In a multiple linear regression model, higher age (p = 0.0015), male sex (p < 0.001), higher BMI (p < 0.001), and higher CHA₂DS₂-VASc score (p = 0.0074) were correlated with a larger difference between the two algorithms, indicating that each variable contributes to the observed deviation.
Conclusion
The results demonstrate that standard P-wave delineation algorithms like ECGDeli systematically underestimate P-wave duration compared to APWD. This discrepancy is most pronounced for prolonged P-waves, which are linked to more advanced stages of AtCM. Therefore an automated algorithm for precise APWD measurement would be beneficial to capture diagnostically valuable late P-wave components, potentially enabling earlier identification of future patients at risk.