Background
Acute heart failure (AHF) remains a significant burden on healthcare systems, necessitating a better understanding of risk factors associated with frequent hospitalizations and adverse outcomes. Clinical and demographic data on in-hospital treatment pathways including procedures, comorbidities and in-hospital mortality continue to be scarce in Germany. We sought to assess risk prediction regarding in-hospital mortality and length of stay in this heterogenous group of patients.
Methods
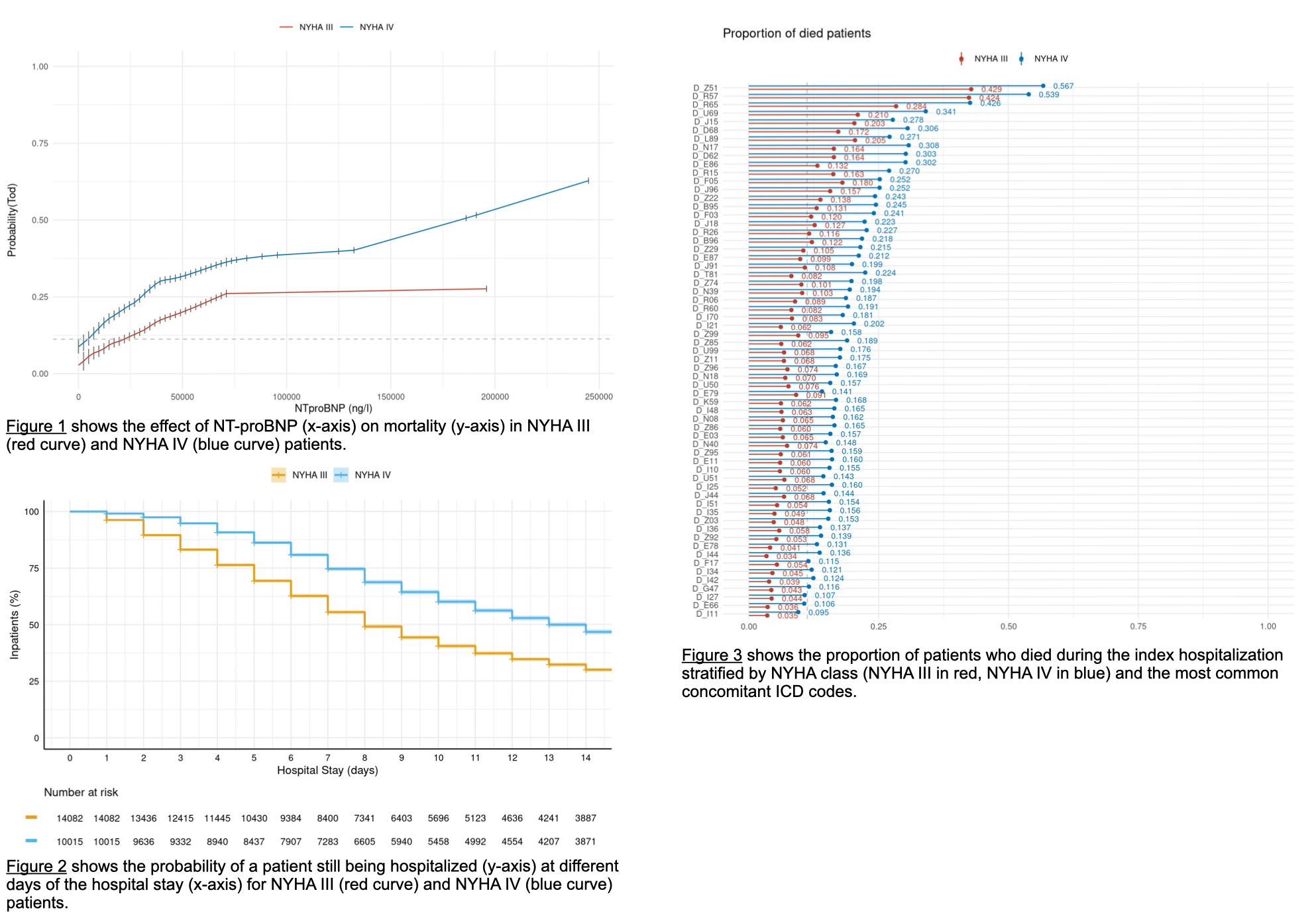
24,097 consecutive patients admitted with AHF were retrospectively analyzed. Patient data, sourced from a comprehensive data warehouse integrating electronic health records with ICD and OPS codes, biometric and biomarker data, among other variables, formed the basis of this investigation. Patients were stratified by New York Heart Association (NYHA) functional classes III and IV. Logistic regression models were employed to calculate mortality trends, while Kaplan-Meier curves were constructed to depict hospital length of stay.
Results
Of the 24,097 patients with AHF, 47% (11,239) were female, the mean age was 77 years. 58% (14,082) were classified as NYHA III. 2.9% (403) of NYHA III patients fulfilled shock criteria, whereas 9.4% (938) of NYHA IV patients suffered from shock. 2.4% of NYHA III patients (341) required mechanical ventilation, compared to 6.9% (693) of NYHA IV patients. Concomitant acute kidney injury was present in 16% (2,275) of NYHA III patients compared to 28% (2,772) of the NYHA IV population.
Among this diverse cohort, an elevated NT-proBNP level demonstrated a significant association with increased mortality. Notably, patients in NYHA class IV exhibited a significantly higher mortality rate compared to their NYHA class III counterparts, even when presenting with similar NT-proBNP levels (figure 1). Furthermore, NYHA class IV patients exhibited a statistically significant higher likelihood of an extended hospital stay (figure 2). Within the deceased cohort, NYHA class IV patients constituted a substantial majority across all explored comorbidities (figure 3), underscoring the heightened risk associated with this advanced heart failure classification.
Conclusions
This study highlights the prognostic significance of biomarker levels and clinical presentation in acute heart failure patients. Elevated NT-proBNP levels were associated with increased mortality, with NYHA class IV patients facing a disproportionately higher risk compared to patients in NYHA class III. Additionally, NYHA class IV patients exhibited a pronounced predisposition to prolonged hospitalization.
While conclusions are to be regarded as hypothesis-generating, these findings underscore the importance of a reliable risk assessment in acute heart failure patients, allowing for targeted interventions and improved patient outcomes.