https://doi.org/10.1007/s00392-024-02526-y
1Ostalb-Klinikum Aalen Innere Medizin II, Kardiologie und Angiologie Aalen, Deutschland; 2Ostalb-Klinikum Aalen Pädiatrie Aalen, Deutschland; 3Universitätsklinikum Giessen und Marburg GmbH Klinik für Innere Medizin - Schwerpunkt Kardiologie Marburg, Deutschland
Background:
Optimizing the recurrence-free outcome of pulmonary vein isolation (PVI) for atrial fibrillation (AF) remains a primary focus in electrophysiology. The use of very High-Power Short-Duration (vHPSD) ablation, utilizing 90W for 4 seconds with the QDOT MICRO™ Catheter (Biosense Webster, Diamond Bar, CA, USA), aims to provide a faster and more effective approach with low complication rates. However, long-term data on recurrence rates remain limited.
Objective:
This study aimed to compare procedural duration, complication rates, and efficacy after 12 months in patients receiving PVI for AF with High-Power Short-Duration (HPSD) ablation (50W for 15 seconds) and vHPSD ablation (90W for 4 seconds).
Methods:
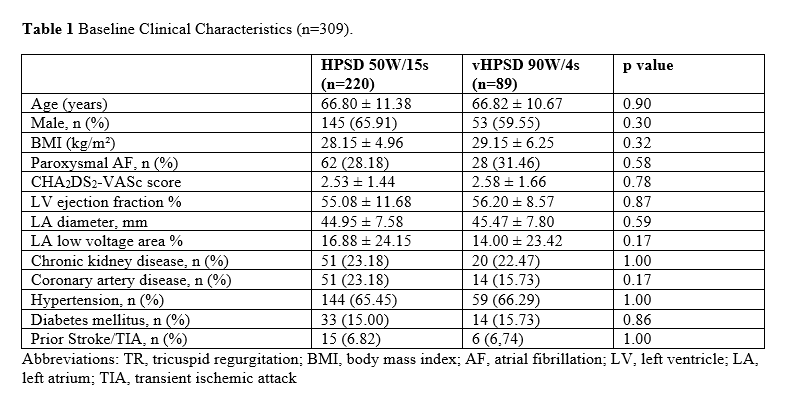
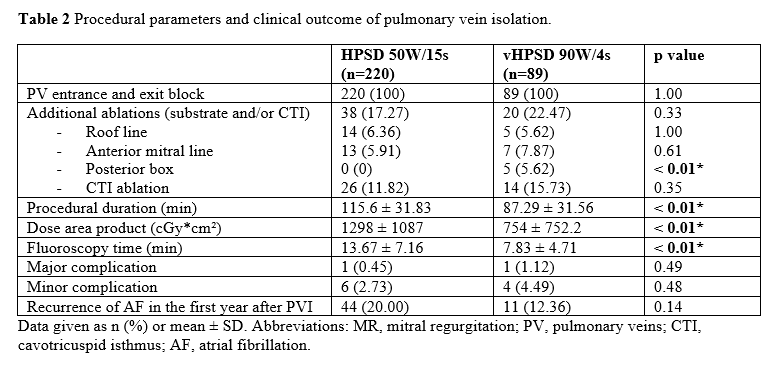
We enrolled 309 consecutive patients with persistent or paroxysmal AF who underwent de novo PVI at our center between 2019 and 2023. Patients receiving HPSD (n=220) were compared to patients undergoing vHPSD (n=89). Additional ablation lines were placed in cases of severe fibrotic substrate, and cavotricuspid isthmus (CTI) ablation was performed if atrial flutter was detected.
Results:
Baseline characteristics were comparable between the groups. The mean procedural time was significantly shorter in the vHPSD group (87.29 minutes) compared to the HPSD group (115.6 minutes) (P<0.01). Entry and exit block were achieved in all patients.
Major complications were rare and did not significantly differ between groups (0.45% in HPSD vs. 1.12% in vHPSD, P=0.49). Minor complications were also similar (2.73% in HPSD vs. 4.49% in vHPSD, P=0.48). Notably, radiation exposure, measured by dose area product, was significantly lower in the vHPSD group (754 ± 752.2 cGy·cm²) compared to the HPSD group (1298 ± 1087 cGy·cm²) (P<0.01). Fluoroscopy time was also reduced in the vHPSD group (7.83 ± 4.71 minutes) compared to the HPSD group (13.67 ± 7.16 minutes) (P<0.01).
Recurrence rates after 12 months, excluding a 90-day blanking period, showed a trend favoring the vHPSD group (12.36%) over the HPSD group (20.00%), although this difference did not reach statistical significance (P=0.14).
In 11 patients with recurrences, re-ablation has been performed to date. Among them, all pulmonary veins (PV) were reconnected in 4 patients, 3 PV were reconnected in 1 patient, and 2 PV were reconnected in 6 patients. No specific pulmonary vein was reconnected more frequently than others.
Conclusion:
vHPSD ablation (90W/4s) for PVI in AF patients offers a significantly faster procedure with lower radiation exposure and comparable safety and efficacy to traditional HPSD ablation (50W/15s). Although the difference in long-term recurrence rates was not statistically significant, the trend suggests a potential benefit of vHPSD in reducing AF recurrence. Further studies with larger cohorts and longer follow-up are warranted to confirm these findings. These results support the clinical utility of vHPSD ablation as a viable option in AF treatment protocols.