1Kerckhoff Klinik GmbH Abteilung für Kardiologie Bad Nauheim, Deutschland; 2Universitätsklinikum Gießen und Marburg GmbH Medizinische Klinik I - Kardiologie und Angiologie Gießen, Deutschland
Introduction
Atrial fibrillation (AF) often coexists with heart failure with reduced left ventricular ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF). In a subset of HFrEF patients arrhythmia induced cardiomyopathy (AIC)/tachycardiomyopathy is present.
The aim of the study was to detect differences in outcome between patients with AIC and HFpEF undergoing cryoballoon pulmonary vein isolation (cryo-PVI) using a propensity score-based model.
Methods
In this retrospective observational study, we analysed persistent AF patients with HFpEF and AIC undergoing cryoballoon ablation between 2014 and 2020. AIC was diagnosed ex juvantibus during the first year after ablation at the 3- and 12-month follow-up when LVEF recovered to > 50% and by more than 10% after ablation and a different aetiology for reduced LVEF was excluded. Propensity score matching was used to pair patients based on their age, sex, CHA2DS2-VASc score and left atrial (LA) area. The primary endpoint was the first documented > 30-s recurrence of atrial arrhythmia after a 3-month blanking period during the one-year follow-up. The secondary endpoints were improvements in NYHA class and reduction of LA area. For identification of independent predictors of atrial arrhythmia recurrence after ablation, univariate and multivariate Cox regression analyses were performed.
Results
Out of 1293 consecutive patients who underwent cryo-PVI, 148 persistent AF patients with HFpEF and 66 patients with AIC were identified. Propensity score matching yielded 46 patients in each group. HFpEF patients were more symptomatic than AIC patients (NYHA: 2.4 +/- 0.5 vs. 2.0 +/- 0,8; p = 0.002). Other baseline characteristics did not differ between the two groups, except LVEF (57 % [IQR: 52-62%] vs. 41% [QR: 35%-45%]; p= 0.002).
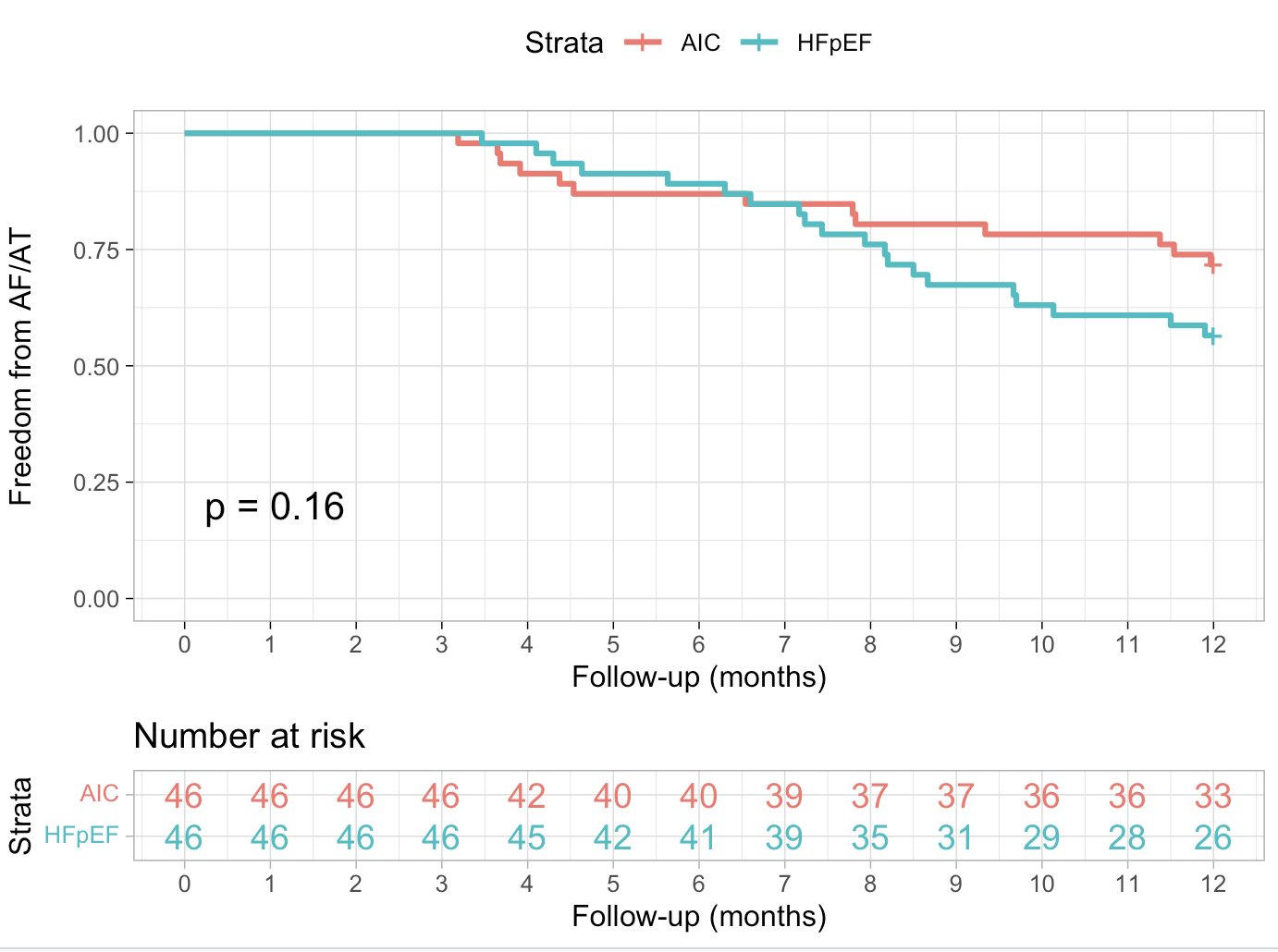
Kaplan-Meier curves (Figure 1) demonstrated no difference in recurrence-free survival rate between the groups during the 12-month follow-up (71.7 % vs. 56.5%, log-rank P = 0.16).
After the 12-month follow-up, the median LA area decreased significantly in the HFpEF group from 25.8 cm2 (IQR: 23.4-29.5 cm2) to 24.6cm2 (IQR: 22.0-29.6 cm2; p = 0.045) and in the AIC group from 26.6 cm2 (IQR: 22.9-31.1 cm2) to 23.0 cm2 (IQR= 18.3-25.2 cm2; p=0.024). At the 12-month follow-up the median LA-area was significantly higher in the HFpEF than in the AIC cohort (p= 0.007). NYHA class improved significantly in both groups from baseline. At the 1-year follow-up NYHA class was similar between both groups (1.6 +/- 0.8 vs. 1.4 +/- 0.6; p = 0.206).
After univariate and multivariate analysis, the following predictors of atrial arrhythmia recurrence were identified: body-mass-index (BMI; HR = 1.082, p = 0.015) and LA area (HR = 1.079, p = 0.003).
Conclusions
Cryoballoon catheter ablation of persistent AF seems to have similar effectiveness on arrhythmia free survival in patients with HFpEF and AIC. NYHA class and LA enlargement improved after ablation in both groups although LA area in HFpEF was higher than in AIC patients at follow-up. BMI and LA area were identified as predictors of arrhythmia recurrence.