Magdalena Baur (Würzburg)1, M. Bauser (Würzburg)1, F. Kraus (Würzburg)2, C. Morbach (Würzburg)1, O. Tuna (Karlsruhe)3, D. D. Pelin (Würzburg)1, F. Sahiti (Würzburg)1, K. Rak (Würzburg)2, S. Frantz (Würzburg)4, S. Störk (Würzburg)1, J. Hoxha (Karlsruhe)3, F. Kerwagen (Würzburg)1
1Universitätsklinikum Würzburg
Deutsches Zentrum für Herzinsuffizienz
Würzburg, Deutschland; 2University of Würzburg
Department of Otorhinolaryngology, Plastic, Aesthetic and Reconstructive Head and Neck Surgery
Würzburg, Deutschland; 3ZANA Technologies GmbH
Karlsruhe, Deutschland; 4Universitätsklinikum Würzburg
Medizinische Klinik und Poliklinik I
Würzburg, Deutschland
Introduction Acute heart failure (AHF) is a life-threatening condition and a frequent reason for hospitalization in Germany. Reliable non-invasive methods for identifying an impeding AHF episode are limited. Smartphone-based voice recordings might facilitate early detection of AHF, but evidence is limited.
Methods The AHF-Voice study is an ongoing monocentric prospective cohort study at the University Hospital Würzburg focusing on the clinical utility of voice alterations in AHF patients. Inclusion criteria are hospitalization for AHF, age ≥18 years, life-expectancy ≥6 months. Exclusion criteria encompass high-urgency listing for heart transplantation, high output HF, cardiogenic shock, and history of vocal fold disease or surgery. Disease history, echocardiogram and routine blood samples were collected during hospitalization. Patients' voice recordings (sustained vowels, standardized text reading, spontaneous speech) were collected at admission and discharge using a specially designed smartphone app, supervised by study staff. For this intermediate analysis, only sustained vowels were used. Voice recordings were pre-processed and voice features extracted using Praat software (version 6.3.13, 31.07.2023, The Netherlands).
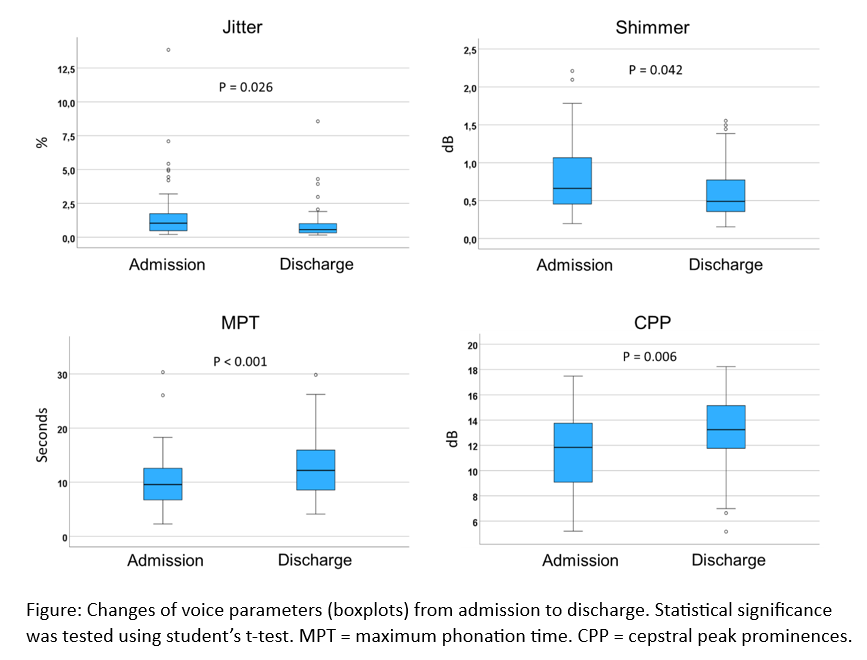
Results Between April 2023 and August 2023, 50 hospitalized patients with AHF were included. Four patients withdrew their consent, and one patient was excluded due to limited voice recording quality. Hence, 90 pairs of voice recordings from admission and discharge were available for analysis. The average age of these patients was 75±10 years, 62% were men, and 49%/ 42%/ 9% were in NYHA class IV/ III/ II at admission, respectively. Left ventricular ejection fraction was reduced in 31%, and preserved in 44% (see Table). Median change of body weight between admission and discharge was -4 kg [-9, -2]. The following voice features were significantly altered between admission and discharge: maximum phonation time, total energy, number of pulses, shimmer, cepstral peak prominences, number of voice breaks, jitter (Figure). No changes were found regarding mean values of pitch and harmonics-to-noise ratio.
Conclusion In this intermediate analysis, a number of easy-to-derive voice features were sensitive to change between admission and discharge for decompensated HF. The clinical utility of vocal biomarkers as a non-invasive indicator for the detection of incipient congestion warrants further research.
|
Baseline characteristics (n=45)
|
|
Male sex
|
28 (62)
|
|
Age (years)
|
75 ± 10
|
|
NYHA functional class
|
|
|
II
|
4 (9)
|
|
III
|
19 (42)
|
|
IV
|
22 (49)
|
|
Type of heart failure
|
|
|
HFpEF
|
20 (44)
|
|
HFmrEF
|
9 (20)
|
|
HFrEF
|
14 (31)
|
|
Length of hospitalization (days)
|
11 ± 6
|
|
History of myocardial infarction
|
14 (31)
|
|
History of diabetes
|
20 (44)
|
|
NT-proBNP (pg/ml)
|
5565 [2997, 13322]
|
|
Sodium (mmol/l)
|
138 ± 4
|
|
Creatinine (mg/dl)
|
1.3 [1.0, 1.7]
|
|
Haemoglobin (g/dl)
|
12 ± 2
|
|
Haematocrit (%)
|
38 ± 7
|
Baseline characteristics in the AHF-Voice study. Data are presented as mean ± SD or median [25th, 75th quartile] for continuous variables or as n (%) for categorical variables.