1Deutsches Herzzentrum der Charité, Charité – Universitätsmedizin Berlin, Campus Virchow Klinikum, Berlin, Germany Klinik für Kardiologie, Angiologie und Intensivmedizin Berlin, Deutschland; 2Charite Universitätmedizin Berlin Institute of Biometry and Clinical Epidemiology. Berlin, Deutschland; 3Charité - Universitätsmedizin Berlin Leiter des Clinical Study Center CVK Berlin, Deutschland
Background:In heart failure with preserved ejection fraction(HFpEF),a clinical condition marked by increased myocardial stiffness, metabolic alterations, and variable afterload,evaluating myocardial work(MW) through non-invasive pressure-strain loop(PSL) analysis from 2D echocardiography(2DE) could offer an accurate assessment of left ventricular(LV) performance,by considering the loading conditions.
Aim:To define MW parameters and to assess their changes with the degree of diastolic dysfunction,biomarkers and symptom severity in HFpEF.
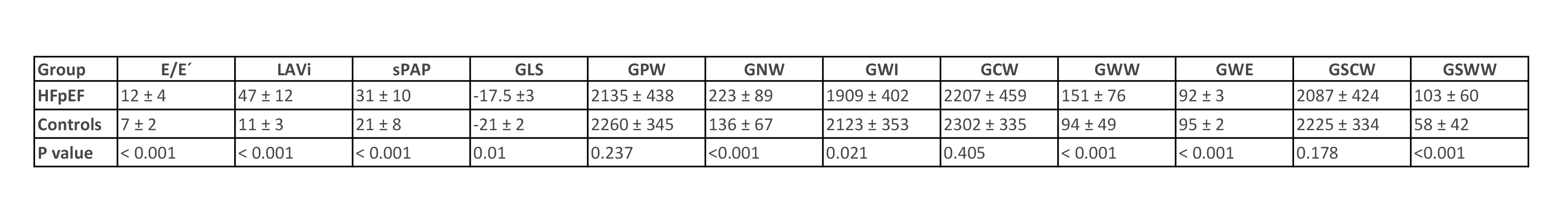
Methods:We prospectively enrolled 40 patients with chronic HFpEF and compared them with 40 sex-matched normal subjects. Clinical, laboratory and 2DE data were collected. We measured LVejection fraction(EF),LV mass index,relative wall thickness(RWT),E/E’ ratio,systolic pulmonary artery pressure(sPAP),left atrial volume index(LAVi),and global longitudinal strain(GLS). We evaluated MW parameters using PSL analysis:global positive work(GPW) defined as the effective energy consumption for LV shortening between mitral valve closure(MVC) and mitral valve opening(MVO);global negative work(GNW) as the energy loss for LV lengthening from MVC to MVO;global work index(GWI) calculated as GPW-GNW, as the total work of the heart;global constructive work(GCW) as the work performed during shortening in systole(effective energy for blood ejection) and lengthening in isovolumetric relaxation(IVR);global wasted work(GWW):work from stretching during systole(energy loss for blood ejection) and shortening during IVR;global work efficiency(GWE) as GCW/(GCW+GWW);global systolic constructive work(GSCW) and wasted work(GWW)as the positive and negative work during LV ejection phase(Fig1).
Results:Median age of the HFpEF group was 76 years(IQR:71-82),all patients were either in NYHA Class II(65%) or NYHA III(35%),49% were male. 84% had a history of hypertension and the mean systolic and diastolic blood pressure were141±17mmHg and82±8mmHg.NtproBNP was 388(IQR:154-521)pg/ml.As expected, all HFpEF patients had LV concentric hypertrophy (LVmass index=129±28g/m2;RWT=0.49±0.04).Compared to controls, E/E´,LAVi and sPAP were significantly higher, whereas GLS was lower in the HFpEF group.MW parameters associated with myocardial energy consumption, that effectively contributes to cardiac output(GPW,GCW,GSCW) were not significant between groups.MW parameters related to the energy loss(GWW,GNW,GSNW) were increased in the HFpEF group, as a consequence of impaired relaxation with prolonged IVR time.As a result, GWE and GWI were reduced, primarily due to an imbalanced increase in GWW and GNW(Fig2).NTproBNP correlated with LAVi(r=0.48,p<0.01) and E/E´(r=0.51,p<0.001).IL6 levels were higher in patients in NYHA III as in NYHA II(p<0.003), being associated with more severe symptoms and poorer patient health status.There was a strong significant negative correlation between IL6 and GWI,GPW,GSCW(r=-0.4,p< 0.05),showing that inflammation plays a role in subclinical systolic dysfunction in HFpEF.
Conclusion:MWE and MWI are decreased,while MWW and GNW are increased in HFpEF, suggesting that elevated wall stress and stiffness contribute to a decrease in contraction efficiency.Thus,in HFpEF a greater energy demand corresponds to a greater energy used, yet this energy is ultimately wasted and fails to convert into an effective cardiac output. Proinflammatory status significantly contributes to subclinical systolic dysfunction in HFpEF, despite a preserved EF.