1Universitätsklinikum des Saarlandes Innere Medizin III - Kardiologie, Angiologie und internistische Intensivmedizin Homburg/Saar, Deutschland; 2Universitätsklinikum des Saarlandes Institut für Rechtsmedizin Homburg/Saar, Deutschland; 3Universität des Saarlandes Anatomisches Institut Homburg, Deutschland
Background: The autonomic nervous system of the heart plays a crucial role in the regulation of cardiac function and cardiovascular homeostasis. However, little data has been published on human coronary innervation so far. Increased sympathetic activity can lead to several cardiovascular diseases, including heart failure, sudden cardiac death, arrhythmias, vasospastic angina, and takotsubo cardiomyopathy. The anatomic characterization and distribution of these perivascular nerves can provide important information on the impact of the autonomic nervous system on myocardial function and perfusion.
Methods: Human hearts were taken from 28 body donors. Tissue samples were excised with adjacent epicardial adipose tissue along the left main coronary artery (LMCA), the left anterior descending artery (LAD), the left circumflex artery (LCx), and the right coronary artery (RCA). Sections were prepared and immunofluorescence staining (S-100, tyrosine hydroxylase) was performed to characterize sympathetic nerve fibers. Coronary innervation was quantitatively analyzed using digital pathology software based on immunofluorescence staining.
Results: A total of 31,009 nerves were analyzed surrounding 100 coronary arteries (LMCA n=21, LAD n=27, LCx n=26, RCA n=26). Comparing the mean nerve fiber diameters of all coronary arteries between the proximal, middle, and distal segments, there is a significant decrease in diameter along the vessel course (64.43±61.32 µm, 50.37±40.62 µm, 39.37±28.57 µm; p<0.001) (Figure 1). Nerves with the largest mean diameter were found along the LMCA (74.51±83.26 µm), followed by nerves around the LAD (59.52±52.01 µm), RCA (47.40±39.55 µm), and LCx (45.04±33.08 µm) (p<0.001). Circumferentially, nerve density was higher in the myocardial tissue half of the coronary arteries (192.85±237.89 nerves/cm²) than in the epicardial tissue half (152.32±196.26 nerves/cm² (p<0.001). Total nerve density was lower in regions with luminal stenosis less than 50% (144.70±145.27 nerves/cm²) compared to regions with higher luminal stenosis. The highest total nerve density in luminal narrowed coronary arteries was found in regions with luminal stenosis greater than 70% (169.66±336,05 nerves/cm² (p=0.02). The mean distance from the nerve to the arterial lumen was smallest around the LMCA (2.88±2.12 mm), followed by the LAD (3.05±2.33 mm), RCA (3.21±2.41 mm), and LCx (3.39±2.86 mm) (p<0.001).
Conclusions: Human coronary arteries are more strongly innervated than previously assumed. The largest nerves are localized at the origin of the left coronary artery and are closest to the arterial lumen. Periarterial nerves of all coronary arteries decrease in diameter along the vessel course and are more densely innervated at the myocardial half of the tissue. In luminal narrowed coronary arteries, periarterial nerve density increases with increasing luminal stenosis. These findings may contribute to the development of new therapeutic strategies for the autonomic modulation of coronary arteries in diseases associated with an increased sympathetic tone.
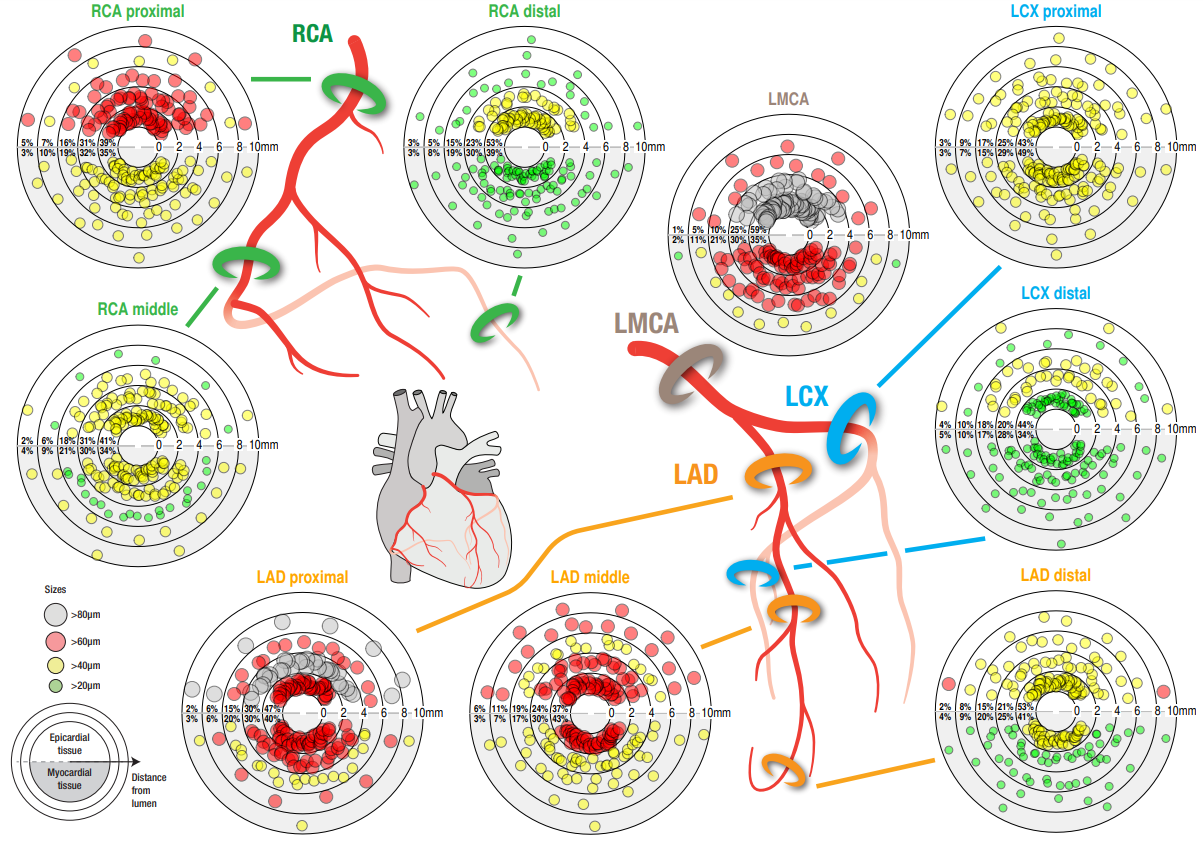
Figure 1: Size and distribution of periarterial nerves according to luminal distance in LMCA, LAD, LCx, and RCA
Figure 1: Size and distribution of periarterial nerves according to luminal distance in LMCA, LAD, LCx, and RCA