1Hospital Clinic University of Barcelona Arrhythmia Section Barcelona, Spanien
Background
Catheter ablation is an effective atrial fibrillation (AF) therapy, but a complex, resource intensive procedure, and it is an increasing challenge for health care systems to accommodate the increasing demand for AF ablation. Same-day discharge (SDD) is an effective way to mitigate this problem by reducing utilization of health care ressources including personell and hospital beds; in fact, few German ablation centers are currently starting to test SDD in selected patients. However, besides structural adaptations, SDD requires more efficient logistics and coordination. Against this background, we established a streamlined SDD program fully coordinated by an advanced practice nurse.
Methods
As dedicated SDD coordinator the advanced practice nurse was in charge of the full SDD protocol, including eligibility, patient flow, in-hospital logistics, patient education, discharge and short-term follow-up. For inclusion, basic home support and accessibility of the hospital within 60 minutes had to be warrented. Patients with LVEF <35% were excluded. Catheter ablation was performed at the operator’s discretion with uninterrupted anticoagulation under general anaesthesia. Ultrasound-guided femoral puncture was at the operator’s discretion for the first 150 SDD patients but became mandatory per protocol for all subsequent patients. Following ablation a figure-of-8 suture and a compressive bandage were employed. Subsequently, patients were monitored at the cardiac short-stay unit for 6 h. Discharge by the SDD coordinator followed a standardized protocol including supervised ambulation, patient education, femoral inspection and echo. On post-ablation days 1 and 3, patients were called by the SDD coordinator to ensure well-being and good aspect of the femoral access site (smartphone foto control). In addition, patients could consult the SDD coordinator via mobile phone any time during working hours. In-person follow-up visits were scheduled at 2 weeks and 3, 6 and 12 months post-ablation.
Results
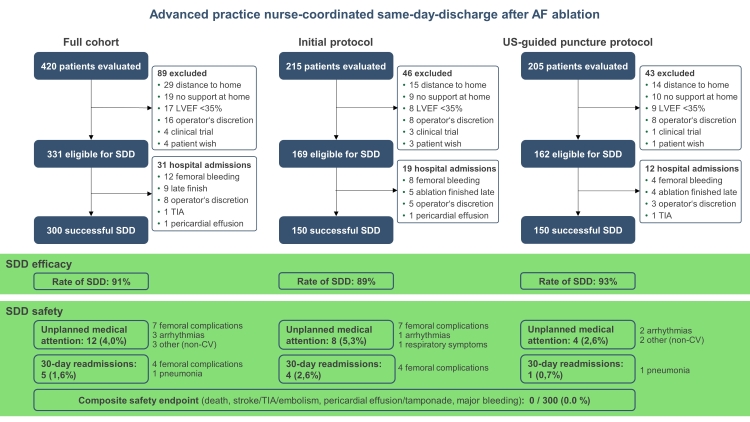
420 consecutive patients were evaluated by the SDD coordinator of whom 331 were eligible for SDD. Reasons for exclusion were living remotely (6.9%), lack of home support (4.5%) or LVEF <35% (4.0%). 300 of the eligible patients (91%) were successfully discharged the same day (Fig.). Rates of unplanned medical attention (4.0%) and 30d-readmission (1.6%) were extremely low compared to previous reports, which may in part be attributed to the patient education and telephone follow-up by the SDD coordinator. Importantly, there was no major post-SDD complication. Unplanned medical attention and hospital readmissions were largely driven by minor femoral access site complications. Of note, those were significantly reduced upon introduction of mandatory ultrasound-guided puncture after the first 150 SDD patients (p=0.0145, Fig. 1).
SDD coordination by the advanced practice nurse streamlined patient flow and in-hospital logistics and significantly reduced the total workload of nursing and medical staff. This resulted in great acceptance of the SDD program and satisfaction both among patients and staff.
Conclusions
Advanced practice nurse-coordinated SDD after AF ablation is safe and efficient. In fact, the position of a dedicated coordinator may be a key in the forthcoming transition of German Hospitals to SDD. Importantly, ultrasound-guided femoral puncture virtually eliminated relevant femoral access site complications and should be a prerequisite for SDD.