https://doi.org/10.1007/s00392-025-02625-4
1Friedrich-Alexander-Universität Erlangen-Nürnberg Medizinische Klinik 2 - Kardiologie und Angiologie Erlangen, Deutschland
Background
The absence of typical symptoms is assumed to delay treatment and consequently result in worse outcomes in patients with non-ST-elevation myocardial infarction (NSTEMI).
Methods
Based on a single-center, all-comers, real-world registry (n=1,192) of patients transferred to the cardiac catheterization laboratory due to a diagnosed NSTEMI, variations and implications of symptoms were analyzed differentiated in the type of myocardial infarction with a focus on patients with type 1 NSTEMI (n=888). Patients were categorized according to their primary symptoms, either in patients with typical symptoms defined as chest pain or pressure, with dyspnea or with atypical symptoms, e.g. epigastric pain. Adverse in-hospital events comprised the composite of in-hospital death, cardiogenic shock, and mechanical ventilation. To investigate mediating effects, causal mediation analysis was conducted.
Results
Overall, typical symptoms were reported as the primary symptom in 77.2%, dyspnea in 14.4%, and atypical symptoms in 8.3% of NSTEMI patients. Patients with type 1 NSTEMI presented more often with typical symptoms than patients with type 2 NSTEMI (81.0 vs. 61.9%, p<0.001). Patients with type 2 NSTEMI more often showed dyspnea (23.7 vs 12.2%, p<0.001) or atypical symptoms (14.4 vs. 6.9%, p < 0.001) than patients with type 1 NSTEMI.
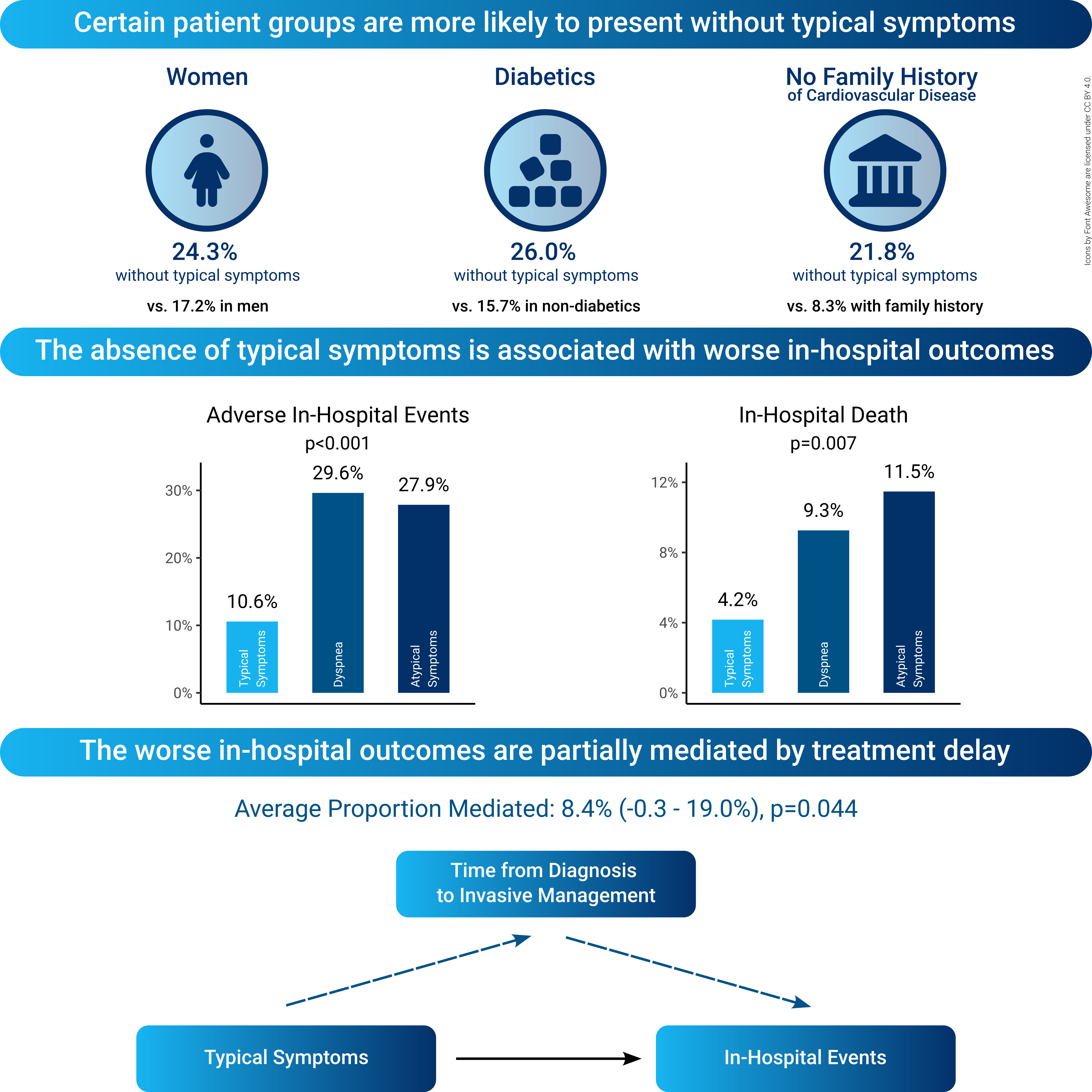
Among 888 patients with type 1 NSTEMI, only 75.7% of women presented with typical symptoms compared to 82.8% of men (p=0.024), only 74.0% of diabetics presented with typical symptoms compared to 84.3% of non-diabetics (p<0.001), and only 78.2% of patients without a family history of premature cardiovascular disease (CVD) presented with typical symptoms compared to 91.7% with a family history (p<0.001). In a multivariable regression analysis including demographics, cardiovascular risk factors, and location and diameter stenosis of the culprit lesion, female sex (p=0.020), diabetes mellitus (p<0.001), and no family history of CVD (p=0.001) were the only independent predictors for the absence of typical symptoms.
In patients with type 1 NSTEMI, the absence of typical symptoms was associated with more adverse in-hospital events (29.6% for dyspnea and 27.9% for atypical symptoms vs. 10.6% for typical symptoms, p<0.001) comprising a higher rate of in-hospital deaths (9.3% for dyspnea and 11.5% for atypical symptoms vs. 4.2% for typical symptoms, p=0.007), cardiogenic shock (28.7% for dyspnea and 23.0% for atypical symptoms vs. 9.3% for typical symptoms, p<0.001), and mechanical ventilation (19.4% for dyspnea and 18.0% for atypical symptoms vs. 4.9% for typical symptoms, p<0.001). The higher rate of in-hospital events in patients without typical symptoms appeared partially mediated (p=0.044) by longer times from diagnosis to invasive management observed among these patients (1410 (IQR: 368-4380) mins for dyspnea and 945 (IQR:241-2210) mins for atypical symptoms vs. 298 (IQR: 121-1060) mins for typical symptoms, p<0.001).
Conclusions
About 20% of patients with NSTEMI present without typical symptoms and about ⅓ of these don’t even perceive dyspnea. The absence of typical symptoms is associated with a higher rate of adverse in-hospital events, which appear to be partially mediated by longer times from diagnosis to invasive management. Therefore, women, diabetics, and patients without a family history of premature CVD may require special attention since they are more likely to present without typical symptoms.
The absence of typical symptoms is assumed to delay treatment and consequently result in worse outcomes in patients with non-ST-elevation myocardial infarction (NSTEMI).
Methods
Based on a single-center, all-comers, real-world registry (n=1,192) of patients transferred to the cardiac catheterization laboratory due to a diagnosed NSTEMI, variations and implications of symptoms were analyzed differentiated in the type of myocardial infarction with a focus on patients with type 1 NSTEMI (n=888). Patients were categorized according to their primary symptoms, either in patients with typical symptoms defined as chest pain or pressure, with dyspnea or with atypical symptoms, e.g. epigastric pain. Adverse in-hospital events comprised the composite of in-hospital death, cardiogenic shock, and mechanical ventilation. To investigate mediating effects, causal mediation analysis was conducted.
Results
Overall, typical symptoms were reported as the primary symptom in 77.2%, dyspnea in 14.4%, and atypical symptoms in 8.3% of NSTEMI patients. Patients with type 1 NSTEMI presented more often with typical symptoms than patients with type 2 NSTEMI (81.0 vs. 61.9%, p<0.001). Patients with type 2 NSTEMI more often showed dyspnea (23.7 vs 12.2%, p<0.001) or atypical symptoms (14.4 vs. 6.9%, p < 0.001) than patients with type 1 NSTEMI.
Among 888 patients with type 1 NSTEMI, only 75.7% of women presented with typical symptoms compared to 82.8% of men (p=0.024), only 74.0% of diabetics presented with typical symptoms compared to 84.3% of non-diabetics (p<0.001), and only 78.2% of patients without a family history of premature cardiovascular disease (CVD) presented with typical symptoms compared to 91.7% with a family history (p<0.001). In a multivariable regression analysis including demographics, cardiovascular risk factors, and location and diameter stenosis of the culprit lesion, female sex (p=0.020), diabetes mellitus (p<0.001), and no family history of CVD (p=0.001) were the only independent predictors for the absence of typical symptoms.
In patients with type 1 NSTEMI, the absence of typical symptoms was associated with more adverse in-hospital events (29.6% for dyspnea and 27.9% for atypical symptoms vs. 10.6% for typical symptoms, p<0.001) comprising a higher rate of in-hospital deaths (9.3% for dyspnea and 11.5% for atypical symptoms vs. 4.2% for typical symptoms, p=0.007), cardiogenic shock (28.7% for dyspnea and 23.0% for atypical symptoms vs. 9.3% for typical symptoms, p<0.001), and mechanical ventilation (19.4% for dyspnea and 18.0% for atypical symptoms vs. 4.9% for typical symptoms, p<0.001). The higher rate of in-hospital events in patients without typical symptoms appeared partially mediated (p=0.044) by longer times from diagnosis to invasive management observed among these patients (1410 (IQR: 368-4380) mins for dyspnea and 945 (IQR:241-2210) mins for atypical symptoms vs. 298 (IQR: 121-1060) mins for typical symptoms, p<0.001).
Conclusions
About 20% of patients with NSTEMI present without typical symptoms and about ⅓ of these don’t even perceive dyspnea. The absence of typical symptoms is associated with a higher rate of adverse in-hospital events, which appear to be partially mediated by longer times from diagnosis to invasive management. Therefore, women, diabetics, and patients without a family history of premature CVD may require special attention since they are more likely to present without typical symptoms.