https://doi.org/10.1007/s00392-025-02625-4
Julius L. Katzmann (Leipzig)1, C. Grellmann (Berlin)2, B. Leppert (Leipzig)3, I. Müller-Kozarez (Leipzig)1, M. Schulz (Berlin)4, U. Laufs (Leipzig)1
1Universitätsklinikum Leipzig
Klinik und Poliklinik für Kardiologie
Leipzig, Deutschland; 2inav – privates Institut für angewandte Versorgungsforschung GmbH
Berlin, Deutschland; 3Gesundheitsforen Leipzig GmbH
Leipzig, Deutschland; 4ABDA-Bundesvereinigung Deutscher Apothekerverbände e. V.
GB Arzneimittel
Berlin, Deutschland
Background and aims
Despite the availability of effective low-density lipoprotein cholesterol (LDL-C)-lowering drugs, only the minority of patients at elevated cardiovascular (CV) risk achieves the guideline-recommended LDL-C treatment targets. This analysis describes current treatment pathways of patients receiving first prescriptions of lipid-lowering therapy (LLT) and the real-world utilization of the first-in-class ATP-citrate lyase inhibitor bempedoic acid (BA) in Germany.
Methods
This analysis was based on the “Deutsche Analysedatenbank für Evaluation und Versorgungsforschung” (DADB), administered by “Gesundheitsforen Leipzig GmbH”, containing health claims data from 15 statutory health insurers, covering about 4.1 million insured persons. For the current analysis, patients ≥ 18 years were included who received a first prescription of LLT between 2016 and 2022 and were at high or very-high CV risk according to the ESC/EAS guidelines 2019. Treatment lines of LLT are presented as Sankey diagrams.
Results
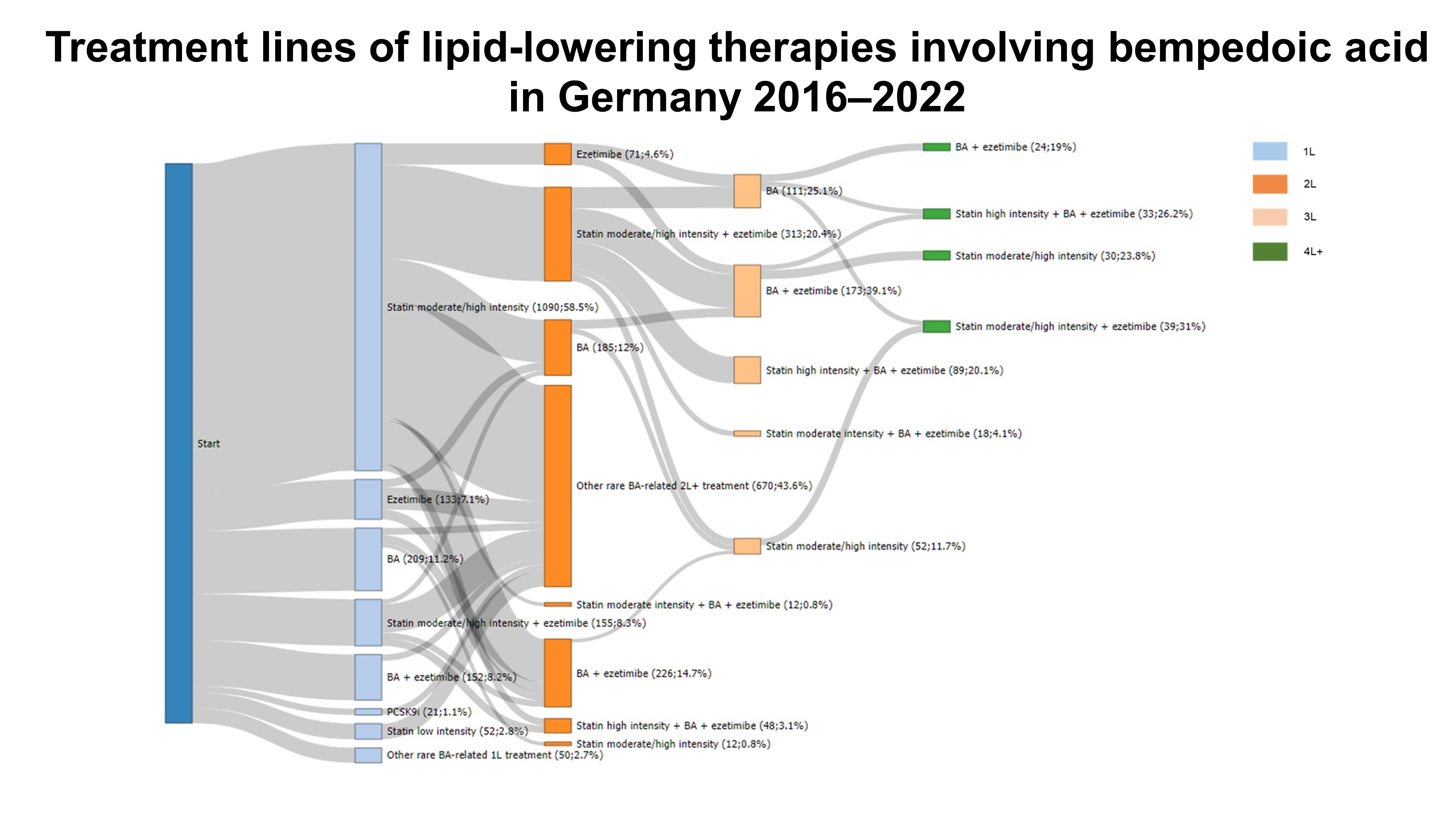
Among 3,487,827 insured persons, 247,529 met the inclusion criteria. The mean age was 64.8 (SD, 11.8) years, 42.5% were female. Coronary artery disease was present in 36.1%, 16.8% had cerebrovascular disease, and 22.8% peripheral artery disease. Hypertension was the most prevalent CV risk factor (87.0%), followed by diabetes (34.1%) and smoking (18.2%). The most frequent first-line LLT were statins in 96.3% of patients, mostly at moderate intensity. Ezetimibe, PCSK9 inhibitors, and BA were first-line LLT in only 0.9%, 0.046% and 0.061% of patients, respectively (Table). Figure 1 shows the treatment lines of all first LLT prescriptions. Only few patients experienced a change in their treatment regimen following LLT initiation. Approximately 10% of patients initially on moderate-intensity statin received a high-intensity statin as second-line LLT. Among patients initiated on moderate- or high-intensity statin, 3.5% received a combination LLT with ezetimibe as second-line treatment. Figure 2 shows treatment lines involving BA. BA was prescribed as first-line LLT as monotherapy in 11.2% among all BA prescriptions, and as combination LLT with ezetimibe in 8.2%. In most cases, BA was prescribed as a second-, third-, or fourth-line add-on treatment.
Conclusions
The most frequently prescribed first-line LLT are statins. Following LLT initiation, changes in LLT were only observed in a minority of patients. Only few patients were escalated to combination LLTs involving BA between Nov. 2020 (market launch of BA) and Dec. 2022. In these cases, BA prescriptions mainly represented second-, third- or fourth-line add-on treatment. Overcoming therapeutic inertia is necessary to exploit the potential of available LLT with proven CV benefit.
Table
|
General
|
|
|
N
|
247,529
|
|
Female (%)
|
42.5
|
|
Age (mean [SD] in years)
|
64.8 (11.8)
|
|
Atherosclerotic cardiovascular disease (%)
|
59.7
|
|
Coronary artery disease
|
36.1
|
|
Cerebrovascular disease
|
16.8
|
|
Peripheral artery disease
|
22.8
|
|
Cardiovascular risk factors and risk classification (ESC/EAS; %)
|
|
|
Hypertension
|
87.0
|
|
Diabetes
|
34.1
|
|
Current smoking
|
18.2
|
|
Cardiovascular risk “high”
|
1.3
|
|
Cardiovascular risk “very-high”
|
97.1
|
|
First-line lipid-lowering therapy (%)
|
|
|
Statin
|
|
|
Low intensity
|
4.7
|
|
Moderate intensity
|
72.6
|
|
High intensity
|
19.0
|
|
Statin (any intensity) + ezetimibe
|
2.7
|
|
Ezetimibe mono
|
0.9
|
|
PCSK9 inhibitor
|
0.046
|
|
Bempedoic acid
|
0.061
|
Figure legend
1L, 2L, …: first line, second line, …; BA: bempedoic acid.
Figure 1
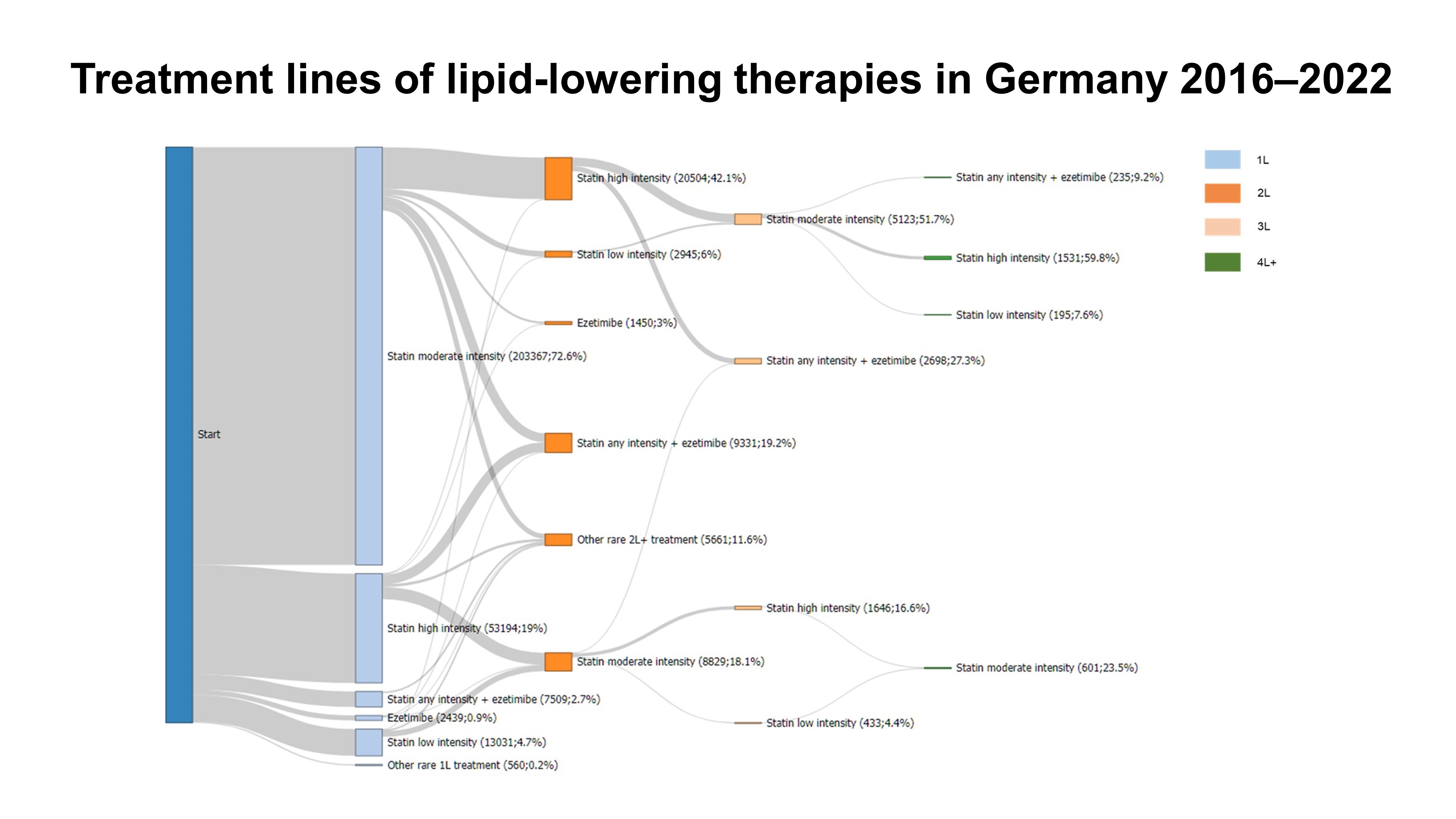
Figure 2