https://doi.org/10.1007/s00392-025-02625-4
1Deutsches Herzzentrum München Klinik für Herz- und Kreislauferkrankungen München, Deutschland
Background
Coronary artery calcification (CAC) is associated with higher rates of adverse cardiovascular events in patients undergoing percutaneous coronary intervention (PCI). Debulking-techniques like rotational atherectomy (rotablation) offer the potential for enhanced lesion preparation which may result in lower stent failure rates in the specific setting of CAC. Whether rotablation improves short- and long-term clinical outcomes of patients with calcified lesions needs to be further investigated.
Objective
To evaluate the efficacy and safety of rotablation based PCI of calcified coronary artery lesions.
Methods
We performed a retrospective analysis of patients who underwent rotablation-based PCI between February 2012 and February 2023 at a German PCI center . Clinical endpoints were all-cause death, target lesion revascularization (TLR), myocardial infarction (MI), probable or definite stent thrombosis after PCI.
Results
679 patients with 1023 lesions with moderate to severe CAC, who underwent rotablation based PCI, were included in this analysis. The mean age was 74.5±8.8 years and 35.8% were diabetics. In 22.4% of cases patients presented with acute-coronary syndromes, 28.0% had prior MI and 20.0% had prior bypass surgery.
At 12 months follow up, 90% of patients were alive. Target lesion revascularization rate was 11.65%. Only 1.05% of TLR events occurred within the first 30 days. Concerning thrombotic events, myocardial infarction rate was 1.94% at 30 days and 2.09% at 1 year, respectively. The rate of definite or probable stent thrombosis was: 2.26% at 30 days and 2.57% at 1 year, respectively.
Conclusion
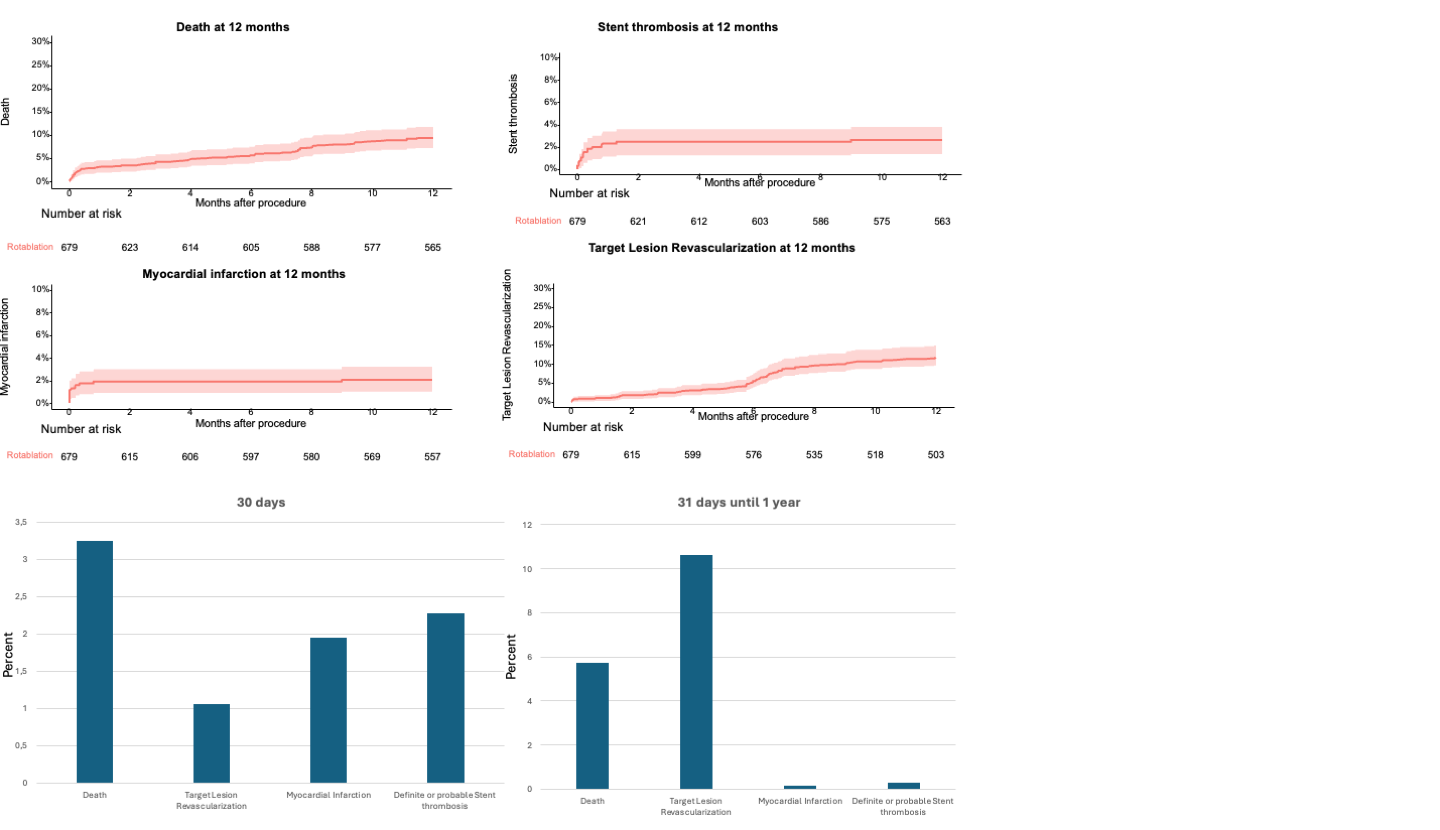
Conclusion
In this large retrospective analysis mortality and revascularization rates remain considerable and may reflect the high risk lesion and patient characteristics of this cohort. Rates of thrombotic events including stent thrombosis and myocardial infarction are high. In the vast majority of cases, thrombotic events occur within the first 30 days after the procedure.