https://doi.org/10.1007/s00392-025-02625-4
1The Heart Center Copenhagen University Hospital Copenhagen, Dänemark; 2Universitätsklinikum Tübingen Innere Medizin III, Kardiologie und Angiologie Tübingen, Deutschland; 3Universitätsklinikum Tübingen Innere Medizin III, Kardiologie und Kreislauferkrankungen Tübingen, Deutschland
Background and Aim
Recent trials found comparable mortality and ischaemic events but reduced bleeding events with single rather than dual antithrombotic therapy (AT) after TAVI. We aimed to investigate whether the implementation of a minimalistic AT approach in real-world practice is associated with lower rates of cardiovascular and bleeding events in TAVI patients.
Methods
This retrospective cohort study utilised TAVI registries from two European hospitals from 2015 to 2021. Patients who were alive after the procedure were stratified according to post-procedural AT with single antiplatelet therapy (SAPT), dual antiplatelet therapy (DAPT), single oral anticoagulation (OAC), dual AT with OAC and SAPT (DAT), and triple therapy (OAC and DAPT). The primary outcomes included major adverse cardiovascular events (MACE) (a composite of death, stroke, and myocardial infarction) and bleeding leading to hospitalisation. Incidence rates per 100 person-years (IR) and adjusted Cox models were made for the primary outcomes comparing SAPT vs. DAPT and OAC vs. DAT.
Results
The study population consisted of 2905 TAVI patients with a mean age of 79.5 years (±7.0) and 45% were female. Of these, 486 (17%) patients were treated with SAPT, 1174 (40%) with DAPT, 313 (11%) with OAC, 895 (31%) with DAT, and 37 (1%) with triple therapy. Switching from a dual to single AT occurred between late 2019 and early 2020 (Figure 1). Patients treated with DAPT and DAT were older and more often treated with percutaneous coronary intervention than those treated with SAPT and OAC, respectively. The number of events and IR for each treatment group are presented in Table 1. At 1-year follow-up, there were no statistically significant differences in the primary outcomes or any individual clinical outcomes between SAPT vs. DAPT or OAC vs. DAT (Table 1). These findings were consistent in sensitivity analyses that excluded patients with prior percutaneous coronary intervention.
Conclusion
A single antithrombotic approach after TAVI was implemented in late 2019. Like prior trials, a single versus dual AT approach was not associated with a higher risk of MACE. The risk of bleeding leading to hospitalisation was comparable between the groups. These findings support current recommendations for a single AT approach after TAVI.
Table 1: Incidence rates per 100 person-years (IR) and adjusted hazard ratios for one-year outcomes according to antithrombotic treatment
Adjusted for age, sex, NYHA class, prior PCI or CABG, self- or balloon-expandable valve, and calendar year.
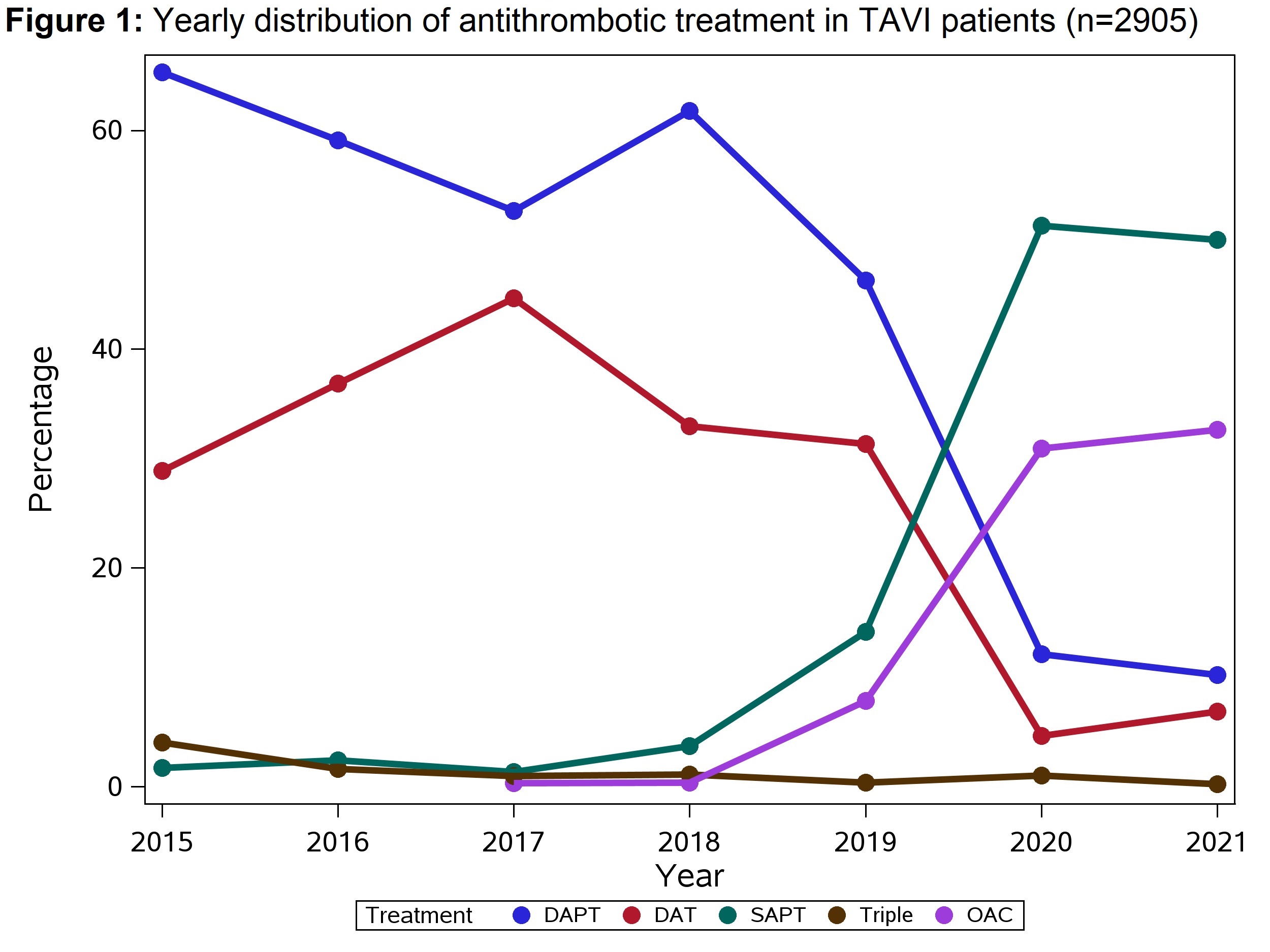
Table 1: Incidence rates per 100 person-years (IR) and adjusted hazard ratios for one-year outcomes according to antithrombotic treatment
| Number of events (IR) | Number of events (IR) | |||||
| One-year outcomes | SAPT (n=486) | DAPT (n=1174) | HR (95% CI) SAPT vs DAPT | OAC (n=313) | DAT (n=895) | HR (95% CI) OAC vs DAT |
| Major adverse cardiovascular events (MACE) | 60 (14.1) | 137 (14.6) | 1.15 (0.76-1.74) | 44 (16.8) | 123 (18.3) | 1.14 (0.71-1.83) |
| Death | 29 (6.2) | 77 (7.4) | 0.75 (0.43-1.33) | 20 (6.9) | 79 (10.5) | 0.83 (0.44-1.56) |
| Stroke | 24 (5.6) | 46 (4.8) | 1.00 (0.64-1.58) | 19 (7.1) | 36 (5.3) | 0.95 (0.57-1.59) |
| Myocardial infarction | 11 (2.5) | 21 (2.2) | 1.04 (0.62-1.74) | 6 (2.2) | 11 (1.6) | 1.10 (0.61-1.99) |
| Bleeding leading to hospitalisation | 50 (12.0) | 102 (11.2) | 0.97 (0.67-1.41) | 34 (13.0) | 81 (12.3) | 0.90 (0.59-1.38) |