https://doi.org/10.1007/s00392-025-02625-4
1Universitätsklinikum AKH Wien Medizinische - Universität Wien Innere Medizin II, Klinische Abteilung für Kardiologie Wien, Österreich; 2Universitätsklinikum Heidelberg Klinik für Innere Med. III, Kardiologie, Angiologie u. Pneumologie Heidelberg, Deutschland; 3Krankenhaus der Barmherzigen Brüder Trier Notfallzentrum Trier, Deutschland
Background:
Insulin-like growth factor binding protein 7 (IGFBP7) is a biomarker associated with heart failure and cardiogenic shock. Here, we aimed to investigate the association of IGFBP7 concentrations and adverse outcomes in patients with out-of-hospital cardiac arrest (OHCA).
Materials and Methods:
IGFBP7 levels were measured on admission and at 24h in OHCA patients included into the ongoing prospective Heidelberg Resuscitation Registry. We used multivariable Cox regression adjusted for age, sex, diabetes status, initial shockable rhythm, bystander cardiopulmonary resuscitation, Simplified Acute Physiology Score II (SAPSII) score and estimated glomerular filtration rate (eGFR) to assess the association between IGFBP7 and all-cause death and neurological dysfunction, defined as a Cerebral performance Category (CPC) > 2.
Results:
In total, we included 165 patients (median age 67 years, 73% male, 21% diabetes, 59% shockable rhythm) with a median follow-up of 16 days. The median IGFBP7 concentrations were 21,405 pg/mL [Interquartile range (IQR) 18,165-25,623] and 23,922 pg/mL [IQR 19822-26417] on admission and at 24 hours, respectively. IGFBP7 levels significantly correlated positively with serum creatinine levels, lactate levels, SAPSII scores, and the Vasoactive-Inotropic Score (VIS) (all P<0.05).
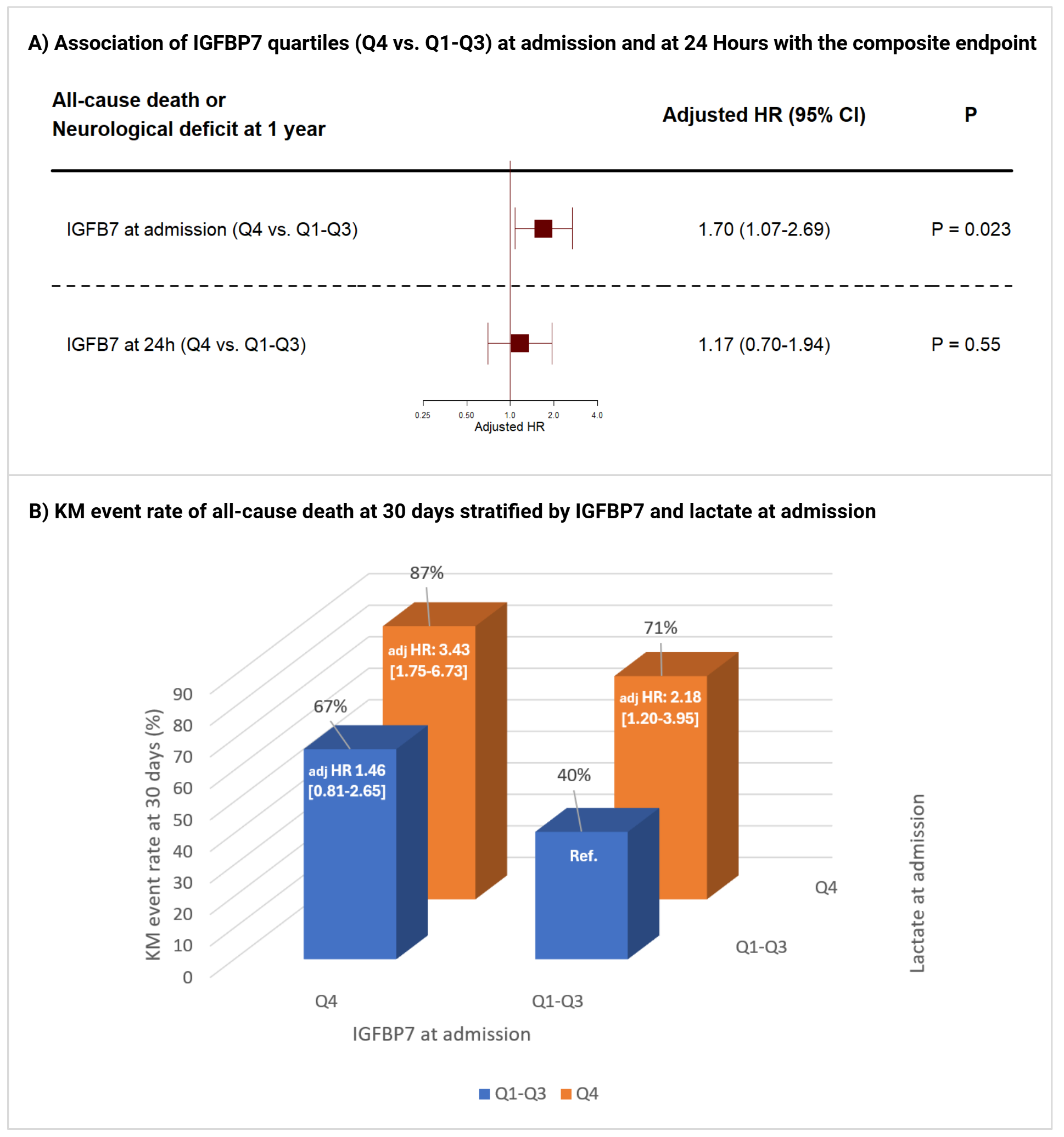
Patients with IGFBP7 concentrations in the top quartile (Q4) on admission (adj HR 1.70 [95% CI 1.07-2.69], P=0.023) had significantly higher risk of death and neurological deficit at 1 year compared to patients in Q1-Q3 (Figure 1A). However, this association was not observed for IGFBP7 concentrations measured at 24h (adj HR 1.17 [95% CI 0.70-1.94], P=0.55).
Furthermore, individuals with both lactate and IGFBP7 in the top quartile upon admission had significantly higher 30-day mortality rates than patients in Q1-Q3 (adj HR for Q4 vs. Q1-Q3, 3.43 [95% CI 1.75-6.73], P<0.001, Figure 1B).
Conclusion:
High IGFBP7 concentrations on admission were strongly associated with increased odds of death and neurological dysfunction in OHCA patients. IGFBP7 may serve as a helpful biomarker for early risk stratification following OHCA.