1Universitätsklinikum Essen Klinik für Kardiologie und Angiologie Essen, Deutschland
Background:
Heart failure with preserved ejection fraction (HFpEF) and atrial fibrillation (AF) are both highly prevalent diseases that commonly coexist, sharing clinical features and pathomechanisms. While prevalence of AF is higher in men compared to women with HFpEF, outcomes appear to be worse in women. However, there are no studies systematically examining gender-specific differences.
Purpose:
Aiming for deeper insights into the effects of gender on clinical outcomes of patients with AF and HFpEF.
Methods:
AF patients with HFpEF treated at the West German Heart and Vascular Center at University Medicine Essen were included. HFpEF was diagnosed according to the current ESC guideline. Outcomes of men and women were compared. The primary endpoint was the time to heart failure hospitalization. Secondary endpoints were the maintenance of sinus rhythm, as well as clinical and functional parameters. Factors related to a primary endpoint event were assessed.
Results:
A total of 161 patients were included in our study (69 male patients, 92 female patients). Assessment of patient characteristics at baseline showed that male patients suffered from coronary artery disease (male: 45/69 patients (65%); female: 45/92 patients (49%); p=0.039), and OSAS (male: 14/69 patients (20%); female: 5/92 patients (5%); p=0.004) significantly more often. After a follow-up of 3 years, occurrence of the primary endpoint event was less frequent in women than in men (Hazard Ratio (HR): 0.61; 95% Confidence Interval (CI): 0.38-0.97; p=0.36; Figure A). There were no significant differences with respect to arrhythmia recurrence. By logistic regression analysis, we identified female sex (HR 0.48; 95%CI: 0.23-0.97; p=0.041), catheter ablation (CA) for AF (HR: 0.26; 95% CI: 0.13-0.53; p<0.001), and a ≥10% decrease in left ventricular mass index (LVMI) (HR:0.66; 95%CI: 0.44-0.98); p=0.041) as preventive factors regarding heart failure hospitalization events. Subgroup analyses showed that while CA for AF only was associated with a primary endpoint reduction in women (HR: 0.39; 95% CI:0.20-0.76; p=0.006), an LVMI improvement of ≥10% was associated with less heart failure hospitalizations in both women (HR:0.47; 95% CI:0.23-0.97; p=0.042) and men (HR: 0.36; 95% CI: 0.18-0.72; p=0.004).
Furthermore, evaluation of functional HFpEF parameters revealed that only in women LVMI (baseline: 111 [99; 133] g/m2; follow-up: 105 [93; 127] g/m2; p=0.006), E/E’ ratio (baseline: 13.0 [10.2; 15.3]; follow-up: 11.5 [8.6; 14.7]; p=0.046), and NT-pro BNP serum levels (baseline: 1367 [352; 3605]; follow up: 987 [438; 2579]; p=0.039) improved at the end of follow-up.
Discussion:
Our study suggests that women with AF and HFpEF have better outcomes as compared to men regarding heart failure hospitalization. We identified a decrease of LVMI by ≥10% and CA for AF to be independently associated with fewer heart failure hospitalizations. While CA only reduced hospitalizations in women, LVMI-decrease improved outcomes of men and women. Only women showed signs of left ventricular reverse remodeling. Consequently, we hypothesize that the gender-specific difference in heart failure hospitalizations is mediated by CA for AF. Supposedly, women are more susceptible for reverse remodeling following CA than men. However, the cause for this phenomenon remains subject to debate and has to be investigated in future studies.
Figure A:
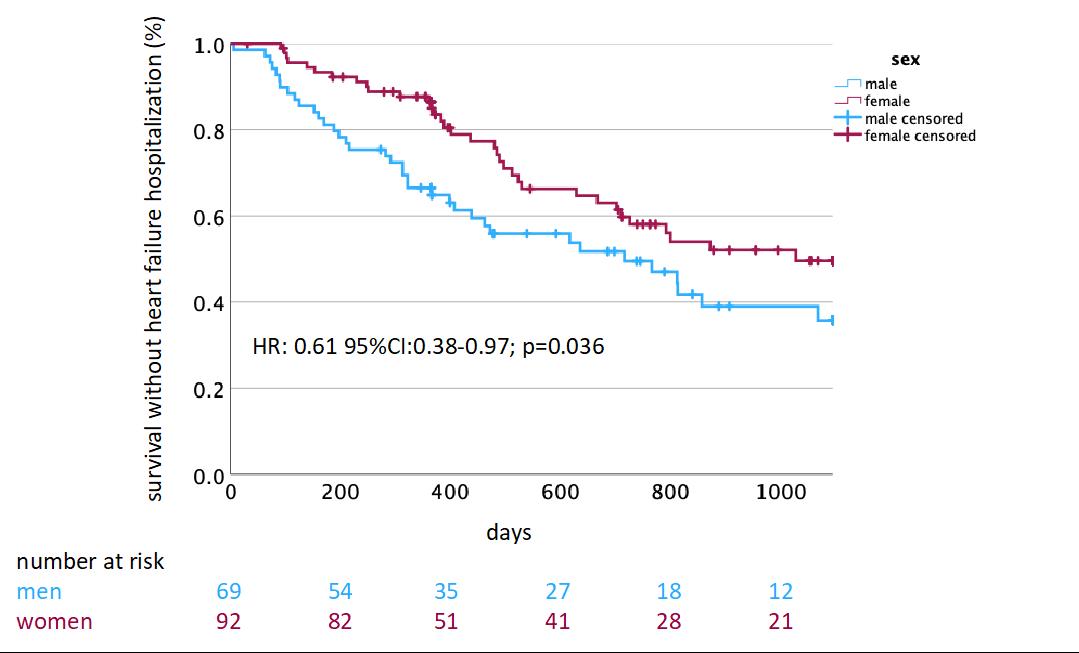
Figure A: