1Klinikum Oldenburg AöR Klinik für Kardiologie Oldenburg, Deutschland
Introduction: Takotsubo Cardiomyopathy is characterized by left ventricular (LV) systolic dysfunction that often mimics a myocardial infarction. It is often triggered by emotional or physical stress and the apex is the most commonly affected region. Variants include midventricular, basal and focal ventricular regions. We report a patient with initial midventricular LV dysfunction and than after six years with a classical, apical systolic akinesia.
Case presentation: In the age of 66 years our patient developed an aortic dissection und received a supracoronary ascending aorta and partial aortic arch prosthetic replacement. Due to prosthetic endocarditis a reoperation with replacement of the aortic root, re-implantation of the coronary ostia and implantation of a freestyle biological aortic valve was performed. The ejection fraction (EF) on echocardiography was 70%.
In the age of 69 years the patient complained about progressive back pain and was admitted to the hospital. The pain increased and radiated into the left sided thorax. Laboratory chemistry revealed an elevated creatininkinase and new negative T waves in the V2 und V3 leads of electrocardiogram (ECG). A cardiac catheterization was done immediately and documented mild coronary arteriosclerosis. Echocardiography and cardiac magnetic resonance imaging (MRI) showed a midventricular LV dysfunction with an EF of 25% (Fig. 1A und 1B). She was discharged with Beta Blocker, Angiotensin Converting Enzyme inhibitor and spironolactone. On follow up the EF improved to 55%.
After six years the then 75-year old patient was admitted to the hospital as an emergency due to sudden onset of severe thoracic pain throughout the chest. In the morning she vomited repeatedly without previous nausea. On admission she had an elevated troponin level of 226 ng/l and increased ST segments in leads V5 and V6 on ECG. Echocardiography demonstrated an EF of 30 % with apical akinesia. This was followed by a cardiac catheterization that revealed again a mild coronary arteriosclerosis with maximal 30% stenosis (Fig. 1E). On cardiac MRI the typical pattern of takotsubo cardiomyopathy with apical LV dysfunction was verified (Fig. 1C und 1D) with no Late Enhancement (Fig. 1F). Therapy at discarge was with verapamil due to asthma bronchiale, Angiotensin Converting Enzyme inhibitor and spironolactone.
Three months after that incidence, we performed a control MRI (Fig. 1G und 1H). The LV function appeared completely normal again without any late enhancement.
Conclusion: The symptoms on both occasions were elevated troponin in the absence of coronary artery disease, pheochromocytoma or myocarditis and fulfill all four criteria of Takotsubo cardiomyopathy. The first presentation was a midventricular dysfunction. This is a rare location and can occur in younger postmenopausal women. It is discussed that in younger age the concentration of adrenoreceptors is midventricular higher than in the apex. Interestingly, six years later the same patient presented with the classical form of takotsubo cardiomyopathy with marked decreased LV function. Among older women the concentration of adrenoceptors is known to be highest in the apex. After both events the patient and the LV function showed a good recovery.
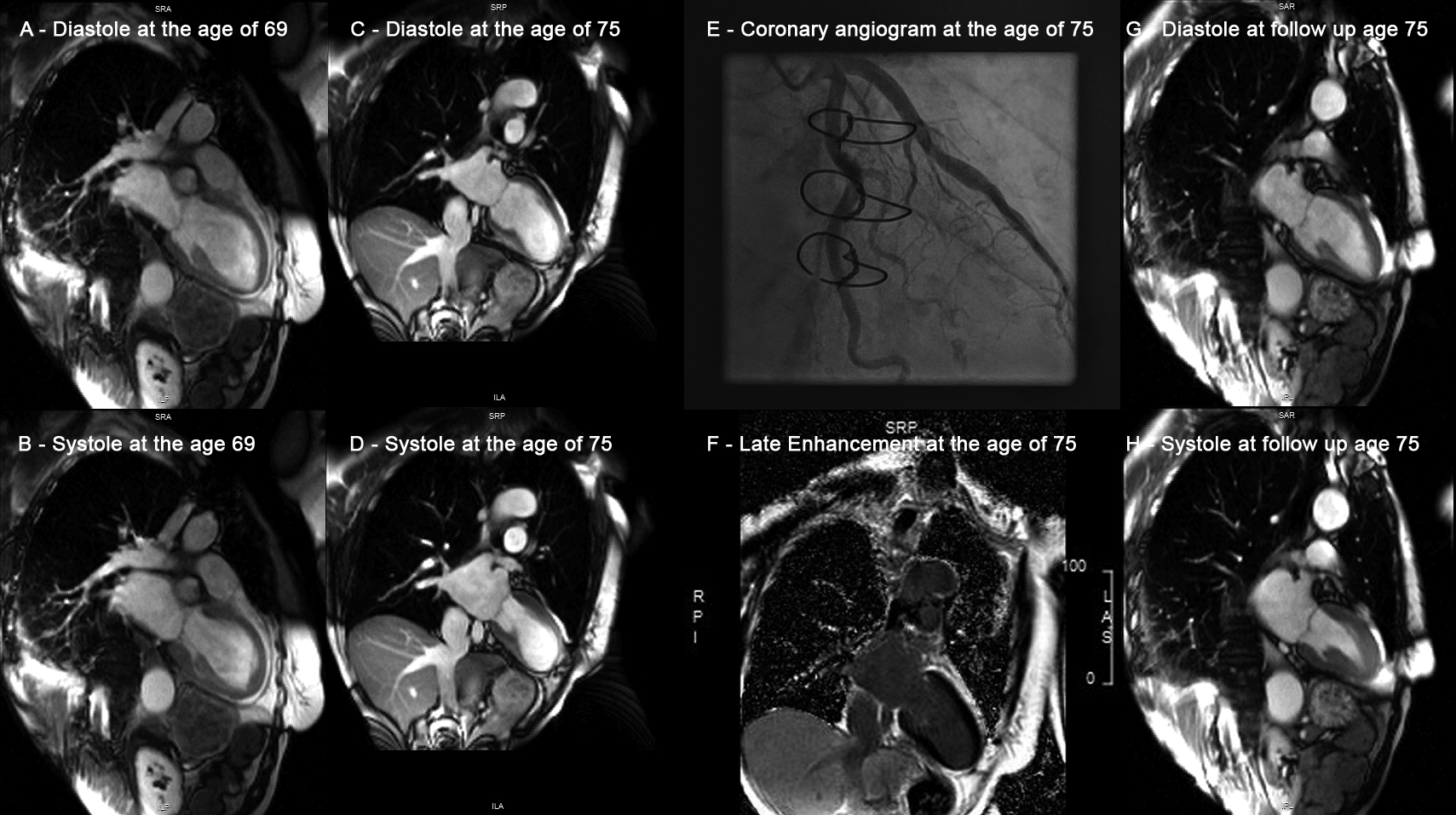
Figure 1: LV function, late enhancement and coronary angiograms at first event (age 69 years) and second takotsubo cardiomyopathy event (age 75 years)
Three months after that incidence, we performed a control MRI (Fig. 1G und 1H). The LV function appeared completely normal again without any late enhancement.
Conclusion: The symptoms on both occasions were elevated troponin in the absence of coronary artery disease, pheochromocytoma or myocarditis and fulfill all four criteria of Takotsubo cardiomyopathy. The first presentation was a midventricular dysfunction. This is a rare location and can occur in younger postmenopausal women. It is discussed that in younger age the concentration of adrenoreceptors is midventricular higher than in the apex. Interestingly, six years later the same patient presented with the classical form of takotsubo cardiomyopathy with marked decreased LV function. Among older women the concentration of adrenoceptors is known to be highest in the apex. After both events the patient and the LV function showed a good recovery.
Figure 1: LV function, late enhancement and coronary angiograms at first event (age 69 years) and second takotsubo cardiomyopathy event (age 75 years)