https://doi.org/10.1007/s00392-025-02625-4
1Medizinische Universität Lausitz-Carl Thiem 1. Medizinische Klinik, Kardiologie, Angiologie Cottbus, Deutschland; 2Medizinische Universität Lausitz-Carl Thiem 1. Medizinische Klinik, Kardiologie, Rhythmologie und Angiologie Cottbus, Deutschland; 3Medizinische Universität Lausitz - Carl Thiem 4. Medizinische Klinik Cottbus, Deutschland
Background:
The Transcatheter Edge-to-Edge Repair (TEER) is an established therapy for patients (pts) with symptomatic severe tricuspid regurgitation and high surgical risk for a conventional surgical procedure. TEE is essential to guide this complex intervention and is considered to be safe, but no larger study investigating the safety of TEE in TEER has been conducted.
Aim of the study:
The aim of our study is to analyse the incidence of periinterventional TEE related minor and major GE-complications during T-TEER procedures even if the pts are asymptomatic, because most of the pts needed immediate oral anticoagulation on top of clopidogrel treatment after the procedure.
Methods:
At our hospital 58 pts with severe tricuspid valve regurgitation (TI) and high surgical risk underwent T-TEER with the TriClip system (Abbott, Chicago, IL, USA).
All interventions were performed under general anesthesia and full heparinisation with an activated clotting time (ACT) of > 250 sec. All pts received routine administration of pantozol 40 mg i.v. twice daily before and after the procedure. One day after the procedure all pts received routinely EGD.
The lesions of the oesophagus were classified after the Forrest classification for upper gastrointestinal bleeding.
Results:
58 pts (age 80.9 ± 0.66 years, 24 male, Euro-Score I 23.9% ±1.8%, EuroScore II 6.8% ± 0.6%, DM (32.8%), Afib (94.8%), NYHA III or IV (91.4%), PPM leads in RV (13.8%) underwent successfully TEER. In total, there was a reduction of mean grade of tricuspid valve regurgitation from 4.1± 0.1 to 1.5 ± 0.08; P < 0.0001. The mean skin-to-skin intervention time was 116.1± 7.13 min.
44 pts (75.9%) had post-TEER EGD and we detected 32 (72.7%) GE-lesions: Forrest Ia 0 (0%), Forrest Ib 2 (4.5%), Forrest II a 0 (0%), Forrest IIb 13 (29.5%), Forrest IIc 3 (6.8%) and Forrest III 5 (11.4%). The residual 9 pts (20.5%) had irrelevant superficial lesions or hematoma. 8 (18.2 %) of these clinically silent GE lesions were treated interventionally by GE-clips. No patients needed blood transfusion despite full oral anticoagulation.
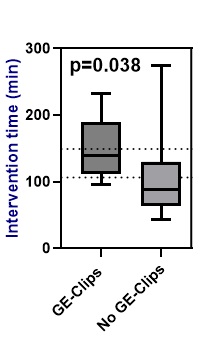
Interestingly there were only 3 (6.8%) lesions found in the stomach although for TEER procedure a gastric view is mandatory and intensively used. Intervention time was significantly longer in pts needing GE-Clip therapy versus pts without GE-Clip therapy : 148.4 ±17.1 min vs 109.9 ± 7.1 min; p=0.038.
A multivariate regression analysis including age, sex, BMI, Euroscore I, Euroscore II and DM showed that only the intervention time is an independent predictor for lesions that needed GE-clip therapy during EGD. (p=0.04).
Conclusion:
Our study shows that major GE injury and bleeding post TEER is rare, but TEE-induced clinically silent lesions of the upper GE-tract requiring interventional GE-clip therapy do occur especially with longer intervention times. The impact of routine EGD following TEER on clinical outcome especially GE-bleeding under oral anticoagulation should be further investigated in prospective randomized trials.