https://doi.org/10.1007/s00392-025-02625-4
1Immanuel Klinikum Bernau Herzzentrum Brandenburg / Kardiologie Bernau bei Berlin, Deutschland; 2Universitätsklinik der Salzburger Landeskliniken Klinik für Innere Med. II, Kardiologie u. intern. Intensivmedizin Salzburg, Österreich
Background
Interventional treatment of tricuspid regurgitation (TR) is a rapidly evolving field but identifying the patients who will benefit most from it remains a challenge. To date, no risk score for transcatheter tricuspid valve interventions (TTVI) has been established or widely used. Leading intervention centers use different risk scores such as the MELD-XI Score (Model for End-Stage Liver Disease, excluding INR), the EuroSCORE II (European System for Cardiac Operative Risk Evaluation) the GLIDE-score, the TRI-score (Tricuspid Regurgitation Impact) and the TRIVALVE-score to predict mortality or rehospitalization. The aim of the study was to compare currently used risk scores regarding their predictive value for rehospitalization or mortality with 12-months after TTVI.
Methods
In this single-center prospective cohort study, data from 60 consecutive patients undergoing “edge to edge” repair (n=47) or “heterotopic minimal invasive tricuspid valve replacement” (n=13) were analyzed. All risk scores (EuroScore II, GLIDE-score, TRIVALVE-score, TRI-score, MELD-XI-score) were obtained before the procedure. Patients were followed up until 12-months after the intervention. Receiver operator characteristics with calculation of the area under the curve (AUC) were performed to show the predictive value of all scores for rehospitalization or mortality. The results of the TRI-score were categorized into low-risk and medium-risk versus high-risk categories using a cut-off value determined by the Youden Index and compared using the chi-square test to evaluate survival rates. A Kaplan-Meier curve was utilized for visualization.
Results
Baseline characteristics of the patients are shown in Table 1. Rehospitalization due to decompensated heart failure occurred in 13 (21.7%) of patients. The 12-months mortality rate was 18.3% (11/60). The predictive values for rehospitalization or mortality is shown in Figure 1. The TRI-score had the best prognostic value with an AUC of 0.76 CI 0.61-0.91; p=0.004. The TRI-score results showed a significant advantage in survival rates (p=0.002) for low- and medium-risk patients compared to the high-risk patients as shown in Figure 2.
Conclusion
In this study, the TRI-score was identified as the best predictive risk score for long-term clinical outcome after TTVI.
Table 1. Baseline characteristics
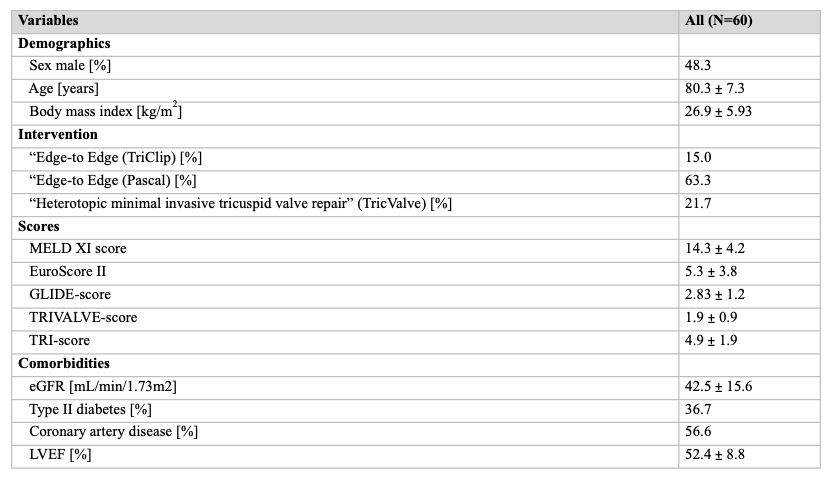
Figure 1. Predictive value of MELD-XI-score (A), TRIVALVE-score (B), TRI-score (C), GLIDE-score (D), EuroScore II (E) for combined endpoint of rehospitalization or death within first 12 month
Figure 2. Kaplan-Meier survival curves of low-/medium risk patients versus high risk patients