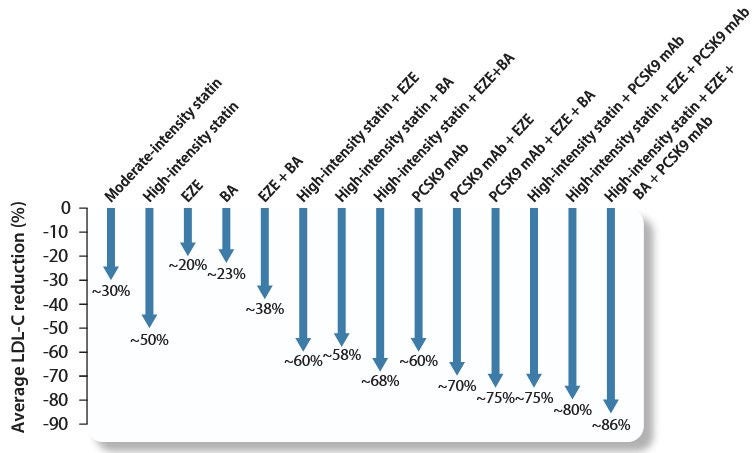
Twenty years ago, the association between intensive lipid-lowering therapy and outcomes after ACS was clearly demonstrated, supporting the principle of “the lower, the better”. Both in the early setting and during the chronic stable phase, LDL-C reduction is a mainstay of management for individuals with ACS. However, the majority of LDL targets are not being achieved with the gradual dose increase recommended in 2019. The principle of “the faster and the lower, the better” has therefore been newly introduced, along with the following recommendations for patients with acute coronary syndrome with and without previous lipid-lowering therapy:
- Individuals undergoing lipid-lowering therapy: Intensification of LDL-C reduction already during ACS hospitalization.
- Treatment-naïve individuals: Start high-intensity statin therapy, possibly in combination with ezetimibe (if it is foreseeable that the LDL-C target cannot be achieved with statin monotherapy).
After starting or intensifying lipid-lowering therapy, LDL-C levels should be checked again within 4–6 weeks. Lifelong lipid-lowering therapy is strongly recommended.